Medical-Surgical Nursing 2 (NURSA 225 01C) - University of Charleton
Medical-Surgical Nursing 2 (NURSA 225 01C) - University of Charleton
Total Questions : 51
Showing 10 questions Sign up for morePlease identify the following rhythm: 
Explanation
Answer and explanation
The correct answer is C. Normal Sinus Rhythm.
Choice A rationale:
Asystole is the absence of all electrical activity in the heart, as evidenced by a flat line on the electrocardiogram (ECG). It is a medical emergency that requires immediate cardiopulmonary resuscitation (CPR) and defibrillation.
Key features of asystole on ECG:
No discernible P waves, QRS complexes, or T waves.
A completely flat or nearly flat line on the ECG tracing.
Choice B rationale:
Atrial flutter is a rapid heart rhythm that arises from abnormal electrical activity in the atria. It is characterized by a sawtooth pattern on the ECG, with atrial rates typically between 250 and 350 beats per minute.
Key features of atrial flutter on ECG:
Absence of distinct P waves, instead replaced by flutter waves (sawtooth pattern).
Regular, rapid atrial rate (typically 250-350 bpm).
QRS complexes may be normal or slightly irregular in appearance.
Choice C rationale:
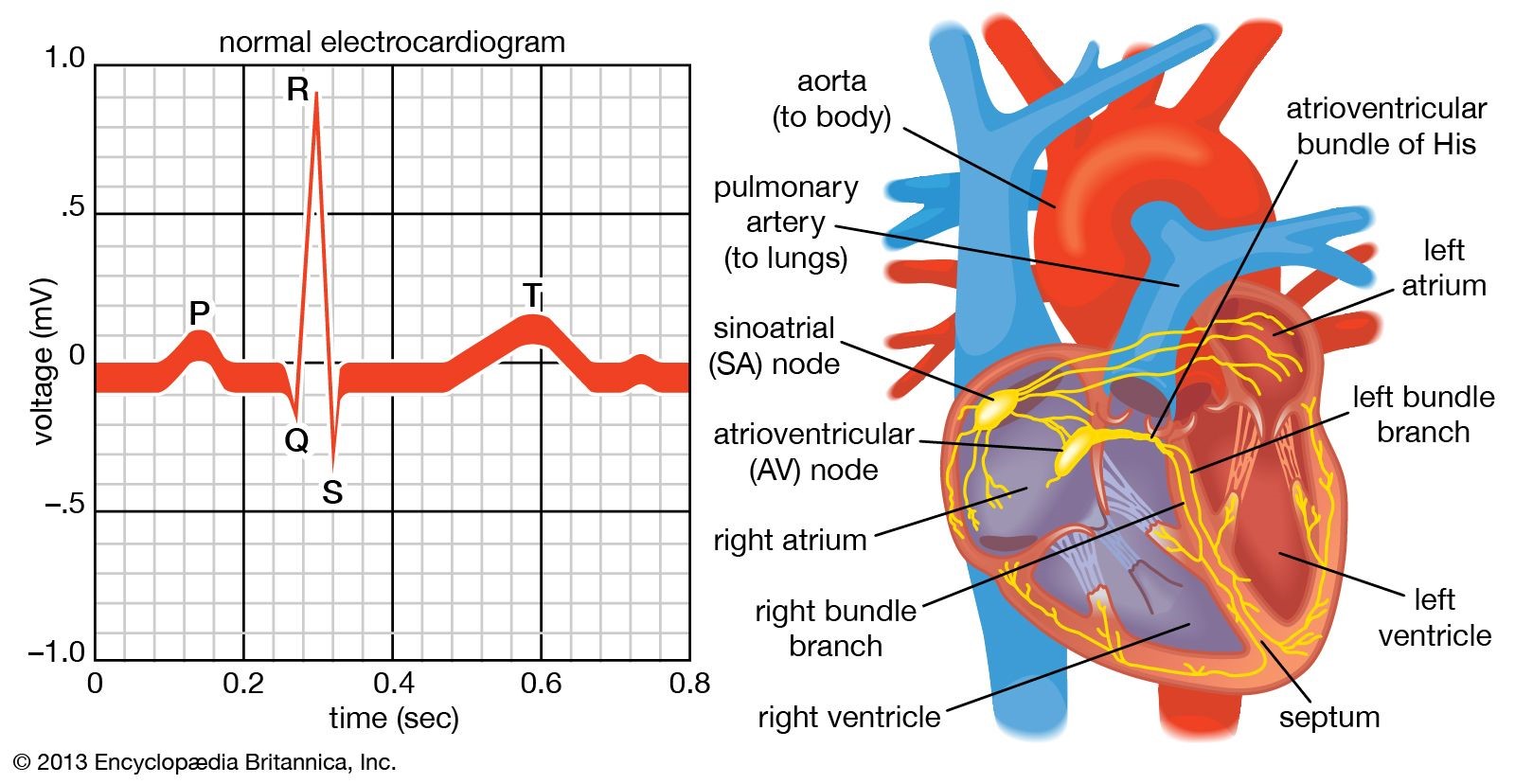
Normal sinus rhythm is the natural, healthy rhythm of the heart. It originates in the sinoatrial (SA) node, the heart's natural pacemaker, and is characterized by a regular rate of 60-100 beats per minute, with consistent P waves, QRS complexes, and T waves on the ECG.
Key features of normal sinus rhythm on ECG:
Presence of distinct P waves, QRS complexes, and T waves.
Regular rhythm with a rate of 60-100 beats per minute.
PR interval (the time between the P wave and QRS complex) is 0.12-0.20 seconds.
QRS duration (the time it takes for the ventricles to depolarize) is less than 0.12 seconds.
Choice D rationale:
Sinus bradycardia is a slow heart rhythm, with a rate below 60 beats per minute. It is often a normal finding in healthy individuals, especially athletes or during sleep. However, it can also be a sign of underlying medical conditions.
Key features of sinus bradycardia on ECG:
Presence of distinct P waves, QRS complexes, and T waves.
Regular rhythm with a rate less than 60 beats per minute.
PR interval and QRS duration are typically normal.
When assisting with defibrillating an adult client who has gone into ventricular fibrillation, what must the nurse do?
Explanation
Choice A rationale:
Calling "all clear" once before discharging the defibrillator is crucial for safety, but it's not the primary action that ensures effective defibrillation.
The purpose of calling "all clear" is to alert everyone in the vicinity to stay clear of the patient and avoid accidental shock.
However, even with a clear announcement, it's essential for the nurse to visually confirm that no one is touching the patient or bed before discharging the defibrillator.
Choice B rationale:
Maintaining firm contact between the paddles and the client's skin is essential for delivering the defibrillation shock effectively.
Here's a detailed breakdown of why this contact is so critical:
Maximizes energy transfer: Firm contact minimizes the impedance (resistance) between the paddles and the skin, allowing for the maximum amount of electrical energy to be transferred to the heart.
Reduces arcing: Arcing occurs when electrical energy jumps through the air instead of passing through the intended path (between the paddles and the heart). This can cause skin burns and reduce the effectiveness of the shock. Firm contact helps prevent arcing by ensuring a direct connection.
Ensures consistent current flow: Consistent contact ensures that the electrical current flows evenly across the chest, reaching all areas of the heart muscle. This increases the likelihood of successful defibrillation.
Minimizes energy loss: Any gaps or poor contact between the paddles and skin can lead to energy loss, reducing the shock's strength and effectiveness.
Choice C rationale:
Sync mode (synchronized cardioversion) is used for specific heart rhythm disturbances, such as atrial fibrillation or atrial flutter, where the shock needs to be timed with the QRS complex on the ECG.
Ventricular fibrillation, however, is a chaotic rhythm without distinct QRS complexes, so sync mode is not appropriate.
Using sync mode in ventricular fibrillation could delay the shock and potentially decrease its effectiveness.
Choice D rationale:
Water is not an appropriate conducting agent for defibrillation.
It can actually increase the risk of burns and decrease the effectiveness of the shock.
Approved conducting agents, such as gel pads or paste, should be used to ensure optimal energy transfer and patient safety.
A client converts from normal sinus rhythm at 80 bpm to atrial fibrillation with a ventricular response at 165 bpm.
Blood pressure is 162/74 mm Hg. Respiratory rate is 20 breaths per minute with normal chest expansion and clear lungs bilaterally.
IV heparin and Diltiazem are given.
What is the main goal of treatment?
Explanation
Choice A rationale:
While maintaining anticoagulation is important in atrial fibrillation to prevent blood clots, it is not the main goal of treatment in this specific scenario.
The client's blood pressure is elevated, suggesting that the rapid heart rate is the more immediate concern.
Additionally, the prompt indicates that heparin has already been administered, addressing the anticoagulation need.
Choice B rationale:
The client's respiratory rate and lung sounds are normal, indicating that oxygenation is not a primary concern at this time.
The fast heart rate is the more pressing issue, as it can lead to decreased cardiac output and potential complications.
Choice C rationale:
Controlling the ventricular heart rate is the main goal of treatment in this case.
Atrial fibrillation with a rapid ventricular response can lead to several detrimental consequences, including:
Decreased cardiac output due to shortened ventricular filling time
Increased myocardial oxygen demand, potentially causing angina or heart failure
Increased risk of stroke or other thromboembolic events
Diltiazem, a calcium channel blocker, is a medication commonly used to slow the heart rate in atrial fibrillation.
By slowing the conduction of electrical impulses through the atrioventricular (AV) node, it effectively reduces the number of impulses that reach the ventricles, thereby controlling the ventricular response.
Choice D rationale:
Decreasing SA node conduction is not a primary goal in this situation.
The SA node is responsible for initiating the normal electrical impulses that trigger heart contractions.
In atrial fibrillation, the electrical activity is chaotic and originates from multiple foci within the atria, rather than the SA node.
Therefore, targeting the SA node would not effectively address the underlying rhythm disturbance.
The nurse is doing discharge teaching with a client who has coronary artery disease.
The client asks why he has to take an aspirin every day if he doesn’t have any pain.
What would be the nurse’s best response?
Explanation
Choice A rationale:
While aspirin can help improve heart function in certain cases, such as by reducing inflammation, it's not accurate to say it directly restores normal heart function. This statement oversimplifies aspirin's mechanism of action and could mislead the client.
It's essential to emphasize aspirin's role in preventing clots, which is the primary reason for its use in coronary artery disease.
Choice B rationale:
Aspirin does not affect the oxygen-carrying capacity of blood. This function is primarily carried out by hemoglobin in red blood cells.
Stating that aspirin increases oxygen-carrying capacity could create misunderstandings about its role in coronary artery disease.
Choice C rationale:
Aspirin does not directly make blood penetrate the heart more freely. Its action primarily involves preventing blood clots from forming within blood vessels.
This statement could lead to a misconception about aspirin's mechanism of action, potentially affecting adherence to treatment.
Choice D rationale:
This is the most accurate and comprehensive response. It directly addresses the client's question and highlights the primary reason for daily aspirin use in coronary artery disease.
Aspirin inhibits platelet aggregation, reducing the risk of blood clots that can obstruct coronary arteries and trigger heart attacks or chest pain.
By preventing these blockages, aspirin can help prevent future cardiovascular events and improve the client's overall health outcomes.
A nurse is describing the process by which blood is ejected into circulation as the chambers of the heart become smaller.
How does the nurse categorize this action of the heart?
Explanation
Choice A Rationale:
Repolarization is a phase in the cardiac cycle that involves the restoration of electrical charges in heart muscle cells, enabling them to prepare for the next contraction. It does not directly refer to the physical contraction and ejection of blood from the chambers.
During repolarization, the heart muscle cells regain their negative electrical charge after depolarization, which triggered the contraction.
Repolarization is essential for maintaining the heart's rhythmic electrical activity and ensuring coordinated contractions.
It does not, however, cause the chambers to become smaller and eject blood, which is the defining feature of systole.
Choice C Rationale:
Diastole is the phase of the cardiac cycle when the heart chambers relax and fill with blood. It is the opposite of systole.
During diastole, the heart muscle relaxes, allowing the chambers to passively expand and collect blood from the veins.
The atrioventricular valves (mitral and tricuspid valves) open during diastole, allowing blood to flow from the atria into the ventricles.
While diastole is crucial for ensuring adequate blood supply to the heart, it does not involve the forceful ejection of blood into circulation that characterizes systole.
Choice D Rationale:
Ejection fraction is a measurement of the heart's pumping efficiency. It represents the percentage of blood that is ejected from the left ventricle with each contraction.
A normal ejection fraction is typically between 55% and 70%.
While ejection fraction is related to systole, it is not a synonym for it. Ejection fraction is a quantitative measure of how well the heart is pumping, while systole refers to the specific phase of the cardiac cycle when contraction and ejection occur.
An older adult client’s assessment reveals the following data: Lying BP 144/82 mm Hg, sitting BP 121/69 mm Hg, standing BP 98/56 mm Hg. What nursing diagnosis should be identified in the client’s plan of care?
Explanation
correct answer is Choice B.
Choice B rationale:
Orthostatic hypotension is a significant drop in blood pressure that occurs when a person stands up from a lying or sitting position. It's characterized by a decrease in systolic blood pressure of at least 20 mmHg or a decrease in diastolic blood pressure of at least 10 mmHg within 3 minutes of standing.
The client's assessment data clearly demonstrates orthostatic hypotension, with a systolic blood pressure drop of 23 mmHg and a diastolic drop of 13 mmHg upon standing.
Orthostatic hypotension is a major risk factor for falls, especially in older adults. This is because the sudden decrease in blood pressure can lead to lightheadedness, dizziness, blurred vision, weakness, and even fainting.
Falls in older adults can result in serious injuries, such as fractures, head trauma, and even death. Therefore, it's crucial to identify and address orthostatic hypotension to prevent falls and their associated complications.
Rationales for other choices:
Choice A: Ineffective breathing pattern is not directly related to orthostatic hypotension. While hypotension can cause shortness of breath in some cases, it's not the primary concern in this scenario.
Choice C: Ineffective role performance can be a consequence of frequent falls, but it's not the most immediate or pressing nursing diagnosis in this case.
Choice D: Risk for imbalanced fluid balance is a potential concern in some cases of orthostatic hypotension, but it's not the most likely diagnosis based on the client's assessment data.
Identify the following rhythm:
Explanation
Atrial fibrillation (AF) is characterized by disorganized electrical activity in the atria, resulting in an irregular and often rapid heart rate.
On an ECG, AF typically presents with absent P waves, irregular R-R intervals, and a rapid ventricular rate (usually >100 beats per minute).
However, the rhythm in the question does not display these characteristic features of AF.
Key features of AF that are absent in the rhythm include:
P waves: AF lacks identifiable P waves, while the rhythm in question may have discernible P waves, although they may be irregular or abnormal.
Regularity: AF is typically irregular, while the rhythm in question is chaotic and without any discernible pattern.
QRS complexes: AF usually has narrow QRS complexes, while the rhythm in question often has wide and bizarre QRS complexes. Choice B rationale:
Ventricular tachycardia (VT) is a rapid heart rhythm originating from the ventricles, with a rate typically exceeding 100 beats per minute.
On an ECG, VT typically presents with wide QRS complexes (>0.12 seconds), a regular or slightly irregular rhythm, and a rate often exceeding 150 beats per minute.
While the rhythm in question is rapid and may have wide QRS complexes, it lacks the regular or slightly irregular pattern often seen in VT.
Key features of VT that distinguish it from the rhythm in question include:
Regularity: VT often has a regular or slightly irregular pattern, while the rhythm in question is chaotic and without any discernible pattern.
QRS morphology: VT typically has monomorphic (uniform) QRS complexes, while the rhythm in question often has polymorphic (varying) QRS complexes.
Choice D rationale:
Premature ventricular contractions (PVCs) are extra heartbeats originating from the ventricles, interrupting the normal heart rhythm.
On an ECG, PVCs appear as early, wide QRS complexes that are often followed by a compensatory pause.
The rhythm in question does not exhibit the characteristic pattern of PVCs, which typically occur as isolated beats or short runs of beats interspersed within a normal rhythm.
Key features of PVCs that are absent in the rhythm include:
Isolation: PVCs typically occur as isolated beats or short runs of beats, while the rhythm in question is sustained and chaotic.
Compensatory pause: PVCs are often followed by a compensatory pause, which is not a feature of the rhythm in question.
The patient’s cardiac rhythm suddenly changes on the monitor.
There are no P waves, instead there are fibrillatory waves before each QRS complex.
How would the nurse interpret the rhythm?
Explanation
Atrial fibrillation (AF) is characterized by the absence of P waves on the ECG, the presence of fibrillatory waves, and an irregularly irregular rhythm. This is due to chaotic electrical activity in the atria, which results in disorganized atrial contractions. The fibrillatory waves, which are often described as "f" waves or "sawtooth" waves, represent the rapid and irregular electrical activity in the atria. They are typically best seen in lead II, V1, or V2 of the ECG.
Here is a more detailed explanation of the key features of AF that support this answer:
Absence of P waves: In normal sinus rhythm, the P wave represents the electrical impulse that originates in the sinoatrial (SA) node and depolarizes the atria. In AF, the SA node is no longer in control of the atrial rhythm, and there is no organized atrial depolarization. As a result, P waves are absent on the ECG.
Presence of fibrillatory waves: The fibrillatory waves seen in AF represent the disorganized electrical activity in the atria. They are typically irregular in amplitude and frequency, and they can vary in appearance from patient to patient.
Irregularly irregular rhythm: The ventricular rhythm in AF is also irregular because the impulses from the atria are not conducted to the ventricles in a regular pattern. This results in an irregularly irregular rhythm, which is a hallmark feature of AF.
Key points to remember:
AF is the most common type of cardiac arrhythmia.
It can be asymptomatic or cause a variety of symptoms, including palpitations, shortness of breath, fatigue, and lightheadedness.
AF is a risk factor for stroke and heart failure.
Treatment for AF may include medications to control heart rate or rhythm, blood thinners to reduce the risk of stroke, and in some cases, procedures to restore normal heart rhythm.
A client with angina has been prescribed nitroglycerin.
Before administering the drug, what potential adverse effects should the nurse inform the client about?
Explanation
Choice A rationale:
Drowsiness and blurred vision are not common adverse effects of nitroglycerin.
While some individuals may experience mild drowsiness, it's not a primary concern.
Blurred vision is not typically associated with nitroglycerin use.
Choice B rationale:
Nervousness and paresthesia (tingling or numbness in the extremities) are not common adverse effects of nitroglycerin.
Some individuals may experience transient anxiety or nervousness, but it's not a characteristic side effect.
Paresthesia is more commonly associated with other medications or conditions.
Choice C rationale:
Throbbing headache and dizziness are the most common adverse effects of nitroglycerin.
They occur due to nitroglycerin's vasodilatory effect, which causes blood vessels to relax and widen.
This can lead to a temporary drop in blood pressure, resulting in headaches and dizziness.
The headaches are often described as throbbing or pulsating, and they typically occur in the frontal or temporal regions of the head.
Dizziness may be mild or severe, and it may be accompanied by lightheadedness or a feeling of unsteadiness.
Choice D rationale:
Tinnitus (ringing in the ears) and diplopia (double vision) are not common adverse effects of nitroglycerin.
They may occur in rare cases, but they are not typically associated with its use.
The ED nurse is caring for a client who has gone into cardiac arrest.
During external defibrillation, what action should the nurse perform?
Explanation
Choice B rationale:
It is crucial to ensure that no one is touching the client during defibrillation to prevent accidental electrical shock to others. The electrical current delivered by the defibrillator is extremely powerful and can cause serious injury or even death if it passes through another person's body. This includes both healthcare professionals and bystanders.
Here are key points to emphasize this rationale:
Electrical conduction: The human body is a good conductor of electricity. If someone is touching the client during defibrillation, the electrical current from the defibrillator can easily pass through their body, potentially causing harm.
Cardiac rhythm disruption: Any contact with the client during shock delivery can interfere with the defibrillator's ability to accurately assess the client's heart rhythm and deliver the appropriate shock. This could potentially worsen the client's condition.
Muscle contractions: The electrical current from the defibrillator can cause involuntary muscle contractions. If someone is touching the client, these contractions could cause them to jerk or move suddenly, potentially causing injury to themselves or others.
Safety guidelines: It is a standard safety guideline in all healthcare settings to clear the area around a client before defibrillation to ensure the safety of everyone involved.
I'll now address the other choices, even though they are not the correct answer, to provide a comprehensive understanding:
Choice A rationale:
While ventilation is important during cardiac arrest, it should be temporarily paused during defibrillation. The chest compressions and electrical shock can cause movement of air in the lungs, which can interfere with the effectiveness of the defibrillation. Additionally, the risk of accidental shock to the person providing ventilation is increased if they are close to the client during defibrillation.
Choice C rationale:
Waiting 3 minutes between shocks is not necessary with modern defibrillators. Current guidelines recommend immediate defibrillation for shockable rhythms such as ventricular fibrillation or pulseless ventricular tachycardia. Delaying defibrillation can decrease the chances of successful resuscitation.
Choice D rationale:
The placement of gel pads is important for effective conduction, but it is not the priority action during defibrillation. Ensuring safety by clearing the area and delivering the shock promptly is more critical in the initial moments of defibrillation.
You just viewed 10 questions out of the 51 questions on the Medical-Surgical Nursing 2 (NURSA 225 01C) - University of Charleton Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



