Postpartum AMD Newborn Care
Postpartum AMD Newborn Care
Total Questions : 41
Showing 10 questions Sign up for moreThe nurse is conducting a prenatal class explaining the various activities that will occur within the first few hours after birth. The nurse determines the session is successful when the couples correctly choose which reason for the use of an antibiotic ointment.
Explanation
Prevent infection of the eyes from vaginal bacteria. This is because some newborns can be exposed to bacteria such as gonorrhea or chlamydia during delivery, which can cause a serious eye infection called gonococcal ophthalmia neonatorum (GON). Applying an antibiotic ointment such as erythromycin or ilotycin can prevent GON and other less severe eye infections by killing the bacteria.
Choice A is not correct because the umbilical cord does not need antibiotic ointment to prevent infection. It should be kept clean and dry until it falls off naturally.
Choice C is not correct because the tear ducts are not affected by vaginal bacteria. They are small tubes that drain tears from the eyes to the nose.
Choice D is not correct because the urethra is not a common site of infection for newborns. The urethra is the tube that carries urine from the bladder to the outside of the body.
A nurse is caring for a postpartum client who saturates a perineal pad in 10 minutes. Which of the following actions should the nurse take first?
Explanation
Massage the client’s fundus. This is because the most common cause of postpartum hemorrhage is uterine atony, which is the failure of the uterus to contract after delivery. Massaging the fundus can stimulate uterine contractions and reduce bleeding by compressing the blood vessels at the placental site.
Choice A is not correct because administering oxytocin is not the first action to take. Oxytocin is a medication that can also help the uterus contract, but it should be given after assessing the uterine tone and bleeding.
Choice B is not correct because observing for pooling of blood under the buttocks is not a priority action. It can help estimate the amount of blood loss, but it does not address the cause of bleeding or stop it.
Choice C is not correct because checking the client’s blood pressure is not the first action to take. Blood pressure can indicate hypovolemia due to blood loss, but it is not a sensitive indicator and may remain normal until a significant amount of blood is lost.
The nurse assesses a postpartum woman's perineum and notices that her lochial discharge is moderate in amount and red. The nurse would record this as what type of lochia?
Explanation
This is because lochia rubra is the first stage of lochia, the vaginal discharge after giving birth. It comprises blood, shreds of fetal membranes, decidua, vernix caseosa, lanugo, and membranes. It is red in color because of the large amount of blood it contains. It lasts 1 to 4 days after birth.
Choice A is not correct because lochia alba is the last stage of lochia. It is whitish or yellowish-white in color and contains fewer red blood cells and more leukocytes, epithelial cells, cholesterol, fat, mucus, and microorganisms. It lasts from the second through the third to sixth weeks after delivery.
Choice B is not correct because there is no such thing as lochia normal. Lochia has three stages: lochia rubra, lochia serosa and lochia alba.
Choice C is not correct because lochia serosa is the second stage of lochia. It is brownish or pink in color and contains serous exudate, erythrocytes, leukocytes, cervical mucus, and microorganisms. It lasts for 4 to 12 days after delivery.
What is the primary rationale for monitoring a new mother every 15 minutes for the first hour after delivery?
Explanation
To check for postpartum hemorrhage.
This is because postpartum hemorrhage is a serious and potentially life-threatening complication that can occur within 24 hours of birth or later. It is defined as a blood loss of more than 500 mL in a vaginal delivery or more than 1000 mL in a cesarean delivery. The most common cause of postpartum hemorrhage is uterine atony, which is the failure of the uterus to contract after delivery. Other causes include lacerations, retained placental fragments, coagulation disorders, and uterine rupture. Monitoring the vital signs, especially blood pressure, and pulse, can help detect signs of hypovolemia due to blood loss. Other signs include pale skin, cold and clammy extremities, delayed capillary refill, decreased urine output, and altered mental status.
Choice B is not correct because determining if the mother's milk is coming in is not the primary rationale for monitoring a new mother every 15 minutes for the first hour after delivery. Milk production usually begins around 48 to 72 hours after delivery and is influenced by hormonal changes, breastfeeding frequency, and maternal health. Although breastfeeding support is important for postpartum care, it is not a priority over checking for postpartum hemorrhage.
Choice C is not correct because monitoring the mother's blood pressure to note any elevations is not the primary rationale for monitoring a new mother every 15 minutes for the first hour after delivery. Elevated blood pressure can indicate gestational hypertension or preeclampsia, which are serious conditions that can affect postpartum women. However, these conditions are more likely to cause symptoms such as headache, blurred vision, epigastric pain, and proteinuria⁴.
Moreover, blood pressure may not be a sensitive indicator of blood loss and may remain normal until a significant amount of blood is lost¹.
Choice D is not correct because answering questions the new parents may have is not the primary rationale for monitoring a new mother every 15 minutes for the first hour after delivery. Although providing education and support to the new parents is an essential part of postpartum care, it is not a priority over checking for postpartum hemorrhage. The new parents may have questions about infant care, feeding, contraception, recovery, and other topics that can be addressed during the postpartum period.
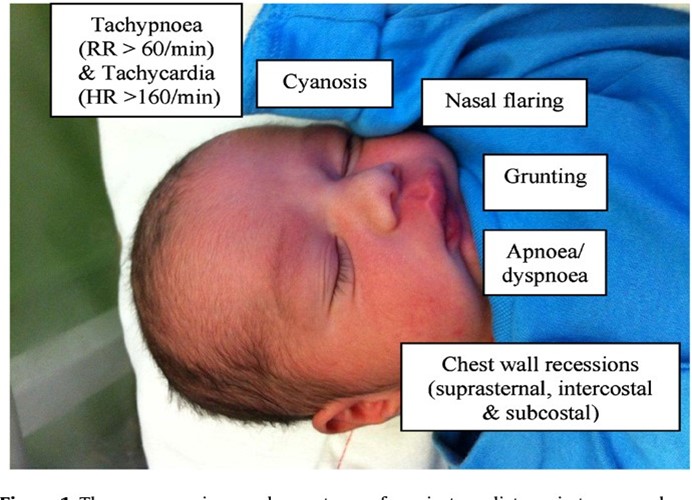
Shortly after delivery, a symptom of respiratory distress in the newborn that should be reported is:
Explanation
Sternal or chest retractions. This is because sternal or chest retractions are a sign of respiratory distress in newborns, which means they are having difficulty breathing. Chest retractions occur when the baby's chest pulls in with each breath, indicating that they are using extra muscles to breathe. This can be caused by various conditions that affect the lungs, such as respiratory distress syndrome (RDS), transient tachypnea of the newborn (TTN), meconium aspiration syndrome (MAS), pneumonia, or congenital heart defects.
 Choice A is not correct because mucus draining from the nose is not a symptom of respiratory distress in newborns. It is normal for newborns to have some mucus in their nose and mouth after birth, which can be cleared by suctioning or wiping.
Choice A is not correct because mucus draining from the nose is not a symptom of respiratory distress in newborns. It is normal for newborns to have some mucus in their nose and mouth after birth, which can be cleared by suctioning or wiping.
Mucus drainage does not interfere with breathing unless it is excessive or thick.
Choice B is not correct because cyanosis of the hands and feet is not a symptom of respiratory distress in newborns. It is normal for newborns to have bluish discoloration of their hands and feet, called acrocyanosis, for the first few days after birth. This is due to immature circulation and does not indicate a lack of oxygen. Cyanosis of the central parts of the body, such as the face, lips, and tongue, is more concerning and should be reported.
Choice C is not correct because irregular heart rate is not a symptom of respiratory distress in newborns. It is normal for newborns to have some variations in their heart rate, especially during sleep cycles. The normal heart rate range for newborns is 100 to 160 beats per minute. A heart rate that is too fast (tachycardia) or too slow (bradycardia) may indicate a problem with the heart or other organs³.
A nurse is collecting data from a newborn and notes a swollen area on the head that does not cross the suture line. The nurse should interpret this finding as which of the following?
Explanation
This is because cephalhematoma is a collection of blood under the scalp that does not cross the suture line. It is caused by trauma to the head during delivery, such as from vacuum extraction or forceps. It usually appears within a few hours or days after birth and resolves within weeks or months.


Choice B is not correct because nevus flammeus is a type of birthmark that is also known as port-wine stain. It is a flat, red, or purple patch of skin that can appear anywhere on the body, but often on the face. It is caused by abnormal blood vessels in the skin and does not go away over time³.
Choice C is not correct because the molding is the temporary change in the shape of the head due to pressure during delivery. It does not cause swelling or bruising and usually resolves within a few days.
Choice D is not correct because caput succedaneum is a type of swelling that affects the scalp and crosses the suture line. It is caused by fluid accumulation under the scalp due to pressure during delivery. It usually appears at birth and goes away within a few days.
A nurse is reviewing the medical record of a client who experienced a vaginal birth 2 hr ago. The nurse should identify which of the following findings places the client at risk for a postpartum hemorrhage.
Explanation
Precipitous birth
This is because precipitous birth, which is defined as a labor that lasts less than three hours from the onset of contractions to delivery, is a risk factor for postpartum hemorrhage. This is because the uterus may not contract well after a rapid delivery, leading to uterine atony and bleeding. Other risk factors for postpartum hemorrhage include uterine overdistension, oxytocin use, placental abruption, placenta previa, infection, coagulation disorders, and previous history of postpartum hemorrhage.
Choice A is not correct because gestational hypertension is not a risk factor for postpartum hemorrhage. It is a condition that causes high blood pressure during pregnancy and can lead to complications such as preeclampsia, eclampsia, and placental abruption³.
Choice B is not correct because small for gestational age newborn is not a risk factor for postpartum hemorrhage. It is a condition that indicates that the baby's growth was restricted in the womb and weighs less than 90% of other babies of the same gestational age. It can be caused by maternal factors, placental factors, or fetal factors⁴.
Choice C is not correct because a two-vessel umbilical cord is not a risk factor for postpartum hemorrhage. It is a condition that occurs when the umbilical cord has only one artery and one vein instead of the normal two arteries and one vein. It can be associated with congenital anomalies, intrauterine growth restriction, and stillbirth.
A nurse is assisting with the care of a newborn following a vaginal delivery. Which of the following actions should the nurse perform first?
Explanation
Clear the respiratory tract. This is because clearing the respiratory tract is the first step in the initial care of a newborn following vaginal delivery. The respiratory tract includes the nose, mouth, and lungs.
Clearing the respiratory tract helps the baby breathe more easily and prevents aspiration of amniotic fluid, blood, or mucus. The nurse can use a bulb syringe or a suction device to gently remove any fluid from the baby's nose and mouth.

Choice B is not correct because drying the infant off and covering the head is not the first action to take. Drying and covering the infant helps prevent heat loss and hypothermia, which are important for newborn care. However, this should be done after clearing the respiratory tract.
Choice C is not correct because stimulating the infant to cry is not the first action to take. Stimulating the infant to cry can help expand the lungs and improve oxygenation, which is also important for newborn care. However, this should be done after clearing the respiratory tract.
Choice D is not correct because clamping the umbilical cord is not the first action to take. Clamping and cutting the umbilical cord separates the baby from the placenta, which is no longer needed after birth. However, this should be done after clearing the respiratory tract.
A woman had a vaginal delivery two days ago and is preparing for discharge. To help prevent postpartum complications, the nurse plans to teach the woman to report any:
Explanation
Fever. This is because fever is a sign of infection, which is a common and potentially serious postpartum complication. Infection can affect various parts of the body, such as the uterus (endometritis), the bladder (cystitis), the breast (mastitis), the wound (wound infection), or the blood (sepsis). Infection can cause symptoms such as fever, chills, pain, foul-smelling discharge, redness, swelling, or warmth at the site of infection.
Choice A is not correct because the change in lochia from red to white is not a sign of postpartum complication. Lochia is the vaginal discharge that occurs after childbirth. It changes color and amount over time, from red to pink to brown to yellow to white. This is a normal process of healing and does not indicate a problem unless the lochia is foul-smelling, heavy, or contains large clots³.
Choice B is not correct because fatigue and irritability are not signs of postpartum complications. Fatigue and irritability are common feelings after childbirth due to hormonal changes, sleep deprivation, physical recovery, and emotional adjustment. They do not necessarily indicate a problem unless they are severe or persistent and interfere with daily functioning or bonding with the baby.
Choice D is not correct because contractions are not signs of postpartum complication. Contractions are normal after childbirth and help the uterus shrink back to its pre-pregnancy size. They are usually mild and subside within a few days. They may be more intense during breastfeeding due to the release of oxytocin, which stimulates uterine contractions.
Following delivery, the nurse's assessment reveals a soft, boggy uterus located above the level of the umbilicus. The appropriate intervention is:
Explanation
Massage the fundus. This is because massaging the fundus (the upper part of the uterus) can help the uterus contract and prevent excessive bleeding after delivery. A soft, boggy uterus indicates uterine atony, which is a failure of the uterus to contract sufficiently after childbirth.
Uterine atony is the most common cause of postpartum hemorrhage, which can be life-threatening if not treated promptly¹².
Choice B is not correct because initiating measures that encourage voiding is not the appropriate intervention for a soft, boggy uterus. A full bladder can interfere with uterine contractions and cause bleeding, so it is important to empty the bladder after delivery. However, this should be done after massaging the fundus.
Choice C is not correct because positioning the patient flat is not the appropriate intervention for a soft, boggy uterus. Positioning the patient flat can increase blood loss and reduce venous return. The patient should be positioned with the head slightly elevated and the legs flexed to improve blood circulation and prevent shock³.
Choice D is not correct because notifying the doctor is not the first intervention for a soft, boggy uterus. Notifying the doctor is important if bleeding persists or worsens despite massaging the fundus. The doctor may order medications or other treatments to stop the bleeding and prevent complications¹.
You just viewed 10 questions out of the 41 questions on the Postpartum AMD Newborn Care Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



