Safe medication quiz
Safe medication quiz
Total Questions : 15
Showing 10 questions Sign up for moreHow can the nurse determine a patient's history of allergies? (Select all that apply.)
Explanation
A. By looking at the MAR: The Medication Administration Record (MAR) is primarily for documenting medications administered, and while it may note some allergies, it is not a comprehensive source for a patient's allergy history.
B. By asking the patient: Directly inquiring about a patient's allergies is one of the most effective methods to gather accurate and specific information. Patients can detail their allergies to medications, foods, and other substances, which might not be documented elsewhere.
C. By looking at the patient's allergy bracelet: An allergy bracelet provides immediate visual identification of known allergies. It serves as an important safety mechanism for healthcare providers to avoid administering any allergens.
D. By looking at the front of the chart or in the patient's electronic health record (EHR): This is a reliable way to find documented allergies. The front of the chart or the EHR often contains essential information about a patient's allergies, which helps inform safe medication administration and treatment planning.
E. By administering a dose and monitoring the patient's response: This method is unsafe and inappropriate. Administering a medication without prior knowledge of allergies could lead to serious and potentially life-threatening reactions. It is critical to know allergy history before any medication administration
The nurse brings the patient's medications but the patient refuses to take them, stating, "I'll take them later. Right now my stomach feels a little upset. Could you please bring me some crackers?" What is the best action the nurse should take? (Select all that apply.)
Explanation
A. Offer the patient some crackers and see if the patient has any medications that could help relieve nausea: This approach addresses the patient's immediate concern about feeling unwell. Offering crackers can help settle the stomach, and checking for any available anti-nausea medication demonstrates attentiveness to the patient's comfort and needs.
B. Leave the medications at the patient's bedside and check on him later: While this action may seem appropriate, it does not ensure that the patient will take the medications later, and it could lead to potential safety concerns if the medications are left unattended.
C. Have the patient take the medications at this scheduled time with a small sip of water: Encouraging the patient to take their medications at the scheduled time with a small sip of water is a good practice. However, given the patient's expressed discomfort, this option may need to be reconsidered based on further assessment of their readiness to take the medications.
D. Document the patient is noncompliant in following the medication regimen: Labeling the patient as noncompliant without fully understanding their reasons could foster a negative therapeutic relationship. It's essential to explore the patient's concerns and address them appropriately before making such a judgment.
E. Lock the patient's medications up temporarily and document the incident: This action could be viewed as punitive and may not support a collaborative approach to care. It is more beneficial to engage with the patient to understand their reluctance to take the medications.
Identify the 6 rights of medication administration.
Explanation
A. The right patient: Identifying the correct patient is crucial to prevent medication errors. This typically involves using at least two identifiers, such as the patient's name and date of birth, to ensure the right person receives the medication.
B. The right MAR: While the Medication Administration Record (MAR) is essential for tracking medication administration, it is not classified as one of the six rights.
C. The right route: Administering medication via the appropriate route (e.g., oral, intravenous) is vital for the drug's effectiveness. Different routes can affect absorption and efficacy, making this a key component of safe medication administration.
D. The right expiration date: Although checking the expiration date is important for safety, it is not part of the core six rights of medication administration.
E. The right health care provider: While appropriate prescribing is important, this does not fall under the six rights of medication administration.
F. The right dose: Confirming the correct dose is essential to avoid potential toxicity or ineffective treatment. Dosage calculations must be precise, considering the patient's age, weight, and clinical condition.
G. The right documentation: Accurate documentation of medication administration is crucial for continuity of care. It helps ensure that all healthcare providers are informed of what medications have been given, thereby preventing duplicate doses or missed medications.
H. The right conversion factor: While conversions may be necessary for dosing, this is not considered one of the six rights.
I. The right medication: Verifying the correct medication is fundamental to patient safety. This involves checking the medication label against the MAR to prevent administering the wrong drug, which could have serious consequences.
J. The right time: Administering medications at the correct scheduled times is essential for maintaining therapeutic drug levels in the body. Timely administration helps ensure that the medication works effectively and enhances patient adherence to their treatment plan.
The patient who is to receive a medication BID will receive the medication:
Explanation
A) Three times a day: This option suggests administering medication at intervals that would total three doses in a 24-hour period. However, "BID" specifically refers to taking a medication twice a day, typically at evenly spaced intervals.
B) Twice a day: The abbreviation "BID" stands for "bis in die," which is Latin for "twice a day." This means that the patient will receive the medication two times within a 24-hour period, often recommended to maintain consistent therapeutic levels.
C) After meals: While some medications are taken after meals for better absorption or to minimize gastrointestinal side effects, the term "BID" does not specify timing relative to meals. Therefore, this option does not accurately describe the frequency of administration.
D) Four times a day: This option indicates administering medication four times within a 24-hour period, which would be represented by the abbreviation "QID" (quater in die) rather than "BID." Thus, it does not align with the definition of taking medication twice daily.
The health care provider has ordered allopurinol 0.05 g PO BID. Drug available: The nurse should give _____ tablet(s) for each dose.
Explanation
A) 1.5: Administering 1.5 tablets of allopurinol would total 150 mg, which exceeds the prescribed dose of 0.05 g (50 mg). Dosing in fractions of tablets can be confusing and is not a typical practice unless the medication is specifically scored for division.
B) 2: Giving 2 tablets would amount to 200 mg, which is significantly higher than the prescribed dose of 50 mg. It's crucial to ensure that the dosage adheres to the healthcare provider's orders to avoid potential toxicity or adverse effects.
C) 0.5: Administering 0.5 tablet (50 mg) is correct. Since the available tablet is 100 mg, cutting it in half will yield the prescribed dose of 0.05 g. This is a safe and effective way to deliver the required medication without exceeding the prescribed limit.
D) 1: One tablet of allopurinol would deliver 100 mg, which is double the prescribed dosage of 0.05 g. It's essential for the nurse to accurately calculate the medication to ensure patient safety and therapeutic effectiveness.
The health care provider has ordered Amikin (amikacin) 500 mg, IM q8h.
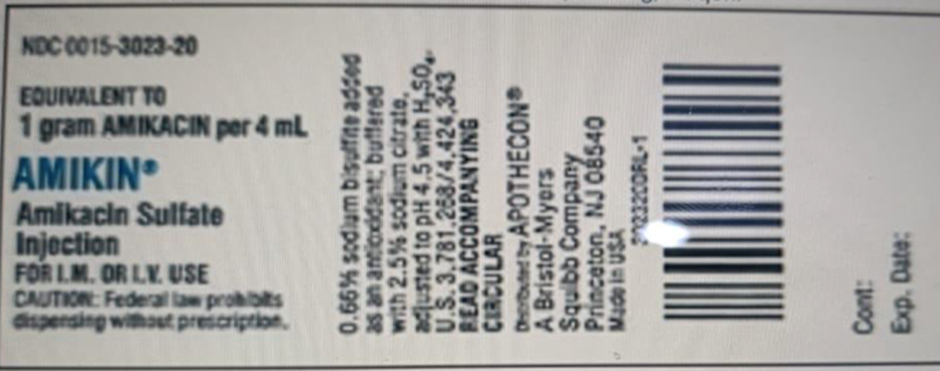
Drug available:
The nurse should give___mL for each dose.
Explanation
A) 1.0: Administering 1.0 mL of Amikin would provide only 250 mg of amikacin, as the concentration is 1 g per 4 mL (or 250 mg per mL). This dosage is insufficient for the ordered dose of 500 mg.
B) 2.0: Administering 2.0 mL of Amikin is correct. With the available concentration of 1 g per 4 mL, 2.0 mL would deliver 500 mg of amikacin (2 mL x 250 mg/mL = 500 mg), fulfilling the healthcare provider's order for the medication.
C) 2.5: Giving 2.5 mL would result in a total of 625 mg of amikacin, which exceeds the prescribed dose of 500 mg. It's critical to adhere to the prescribed dosage to prevent potential toxicity and ensure patient safety.
D) 1.5: Administering 1.5 mL would provide 375 mg of amikacin, which is still less than the required 500 mg. Accurate dosing is essential in achieving the therapeutic effect and avoiding complications.
The health care provider has ordered prochlorperazine (Compazine) 2.5 mg IM q4h prn. The medication available is Compazine 5 mg/mL. The nurse should give ___ mL for each dose.
Explanation
A) 2: Administering 2 mL of Compazine would provide a total dose of 10 mg (since the concentration is 5 mg/mL), which exceeds the ordered dose of 2.5 mg. This option is incorrect as it would administer too much medication.
B) 1.5: This option suggests giving 1.5 mL, which would equate to 7.5 mg (1.5 mL x 5 mg/mL). This dosage also exceeds the ordered 2.5 mg and is therefore not appropriate.
C) 1: Administering 1 mL would deliver 5 mg of Compazine. This amount is higher than the prescribed 2.5 mg and is not the correct dose.
D) 0.5: This option is correct. Administering 0.5 mL of Compazine would provide a dose of 2.5 mg (0.5 mL x 5 mg/mL). This matches the ordered dosage perfectly, ensuring that the patient receives the correct amount of medication.
The health care provider has ordered Amoxil (amoxicillin) 0.05 g, PO tid.

Drug available: The nurse should give ____ mL for each dose.
Explanation
A) 1.5: Administering 1.5 mL of Amoxil would provide 37.5 mg of amoxicillin (125 mg per 5 mL translates to 25 mg per mL), which is insufficient to meet the ordered dose of 0.05 g (50 mg). Accurate dosing is essential for effective treatment.
B) 0.5: Giving 0.5 mL would result in only 12.5 mg of amoxicillin, which is significantly below the prescribed dose of 0.05 g. It's crucial to ensure the dose administered aligns with the healthcare provider's orders to achieve the desired therapeutic effect.
C) 2: Administering 2 mL of Amoxil is correct. At a concentration of 125 mg per 5 mL, this dosage provides 50 mg of amoxicillin (2 mL x 25 mg/mL = 50 mg), which meets the prescribed order and ensures proper treatment.
D) 1: One mL would deliver 25 mg of amoxicillin, which is still inadequate compared to the required dose of 50 mg. Proper dosing ensures the medication's efficacy while minimizing the risk of resistance and treatment failure.
What is the best way for nurses to prevent medication errors?
Explanation
A) Use an automated medication dispensing system: While automated systems can enhance efficiency and reduce the risk of errors, they are not foolproof. Errors can still occur due to incorrect entries or malfunctions, so reliance solely on technology without further precautions may not be sufficient.
B) Avoid distractions and take time to prepare medications: Reducing distractions is important for maintaining focus during medication preparation. However, it is just one aspect of a comprehensive approach to medication safety. This practice alone does not encompass the necessary protocols that ensure the correct medication is administered.
C) Adhere to the 6 rights of medication administration: Following the 6 rights—right patient, right drug, right dose, right route, right time, and right documentation—is the most effective strategy for preventing medication errors. This systematic approach provides a framework for nurses to ensure accuracy and accountability in every medication administration.
D) Only give medications to patients who are alert and oriented: While it’s important to assess a patient's alertness before administering medications, this criterion alone does not address the various factors that can lead to medication errors. Patients may require medications even when not fully alert, and it is the nurse's responsibility to ensure safety through proper protocols rather than simply limiting administration based on alertness.
If the patient refuses a medication, what should the nurse do? (Select all that apply.)
Explanation
A) Notify the health care provider: It is essential to inform the healthcare provider if a
patient refuses a medication. This allows for a reassessment of the patient's treatment plan and ensures that any necessary follow-up or adjustments can be made based on the patient's refusal.
B) Determine the reason for refusal: Understanding why a patient refuses medication is crucial. It may be due to side effects, lack of understanding, personal beliefs, or concerns about the medication. Gathering this information can help the nurse address the patient’s concerns and educate them appropriately.
C) Administer the dose when the next dose is due: Administering a medication that the patient has refused would violate their rights and could be considered coercive. The patient has the right to refuse treatment, and the nurse should respect that decision rather than attempt to administer it later without consent.
D) Document the reason for refusal in the patient's health record: Accurate documentation is vital in healthcare. Recording the patient's refusal and the reason for it in their health record ensures continuity of care and provides information for other healthcare team members regarding the patient's preferences and concerns.
E) Mix it in a small amount of their food: This action is inappropriate and unethical. Coercively administering medication without the patient's consent undermines their autonomy and trust in the healthcare system. The nurse should always respect the patient’s right to refuse medication.
You just viewed 10 questions out of the 15 questions on the Safe medication quiz Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



