A 31-year-old male patient with burn injuries is admitted to the burn unit. Which priority does the nurse anticipate within the first 24 hours?
Sterile dressing changes
Emotional support
Fluid resuscitation
Range-of-motion exercises
The Correct Answer is C
In the initial 24 hours after burn injury, fluid resuscitation is a critical priority in the management of burn patients. Burn injuries can lead to significant fluid loss, both locally at the burn site and systemically due to increased capillary permeability. Fluid resuscitation aims to restore and maintain adequate intravascular volume, ensuring sufficient tissue perfusion and organ function.
The Parkland Formula is commonly used to guide fluid resuscitation in burn patients. It involves calculating the total volume of fluid needed in the first 24 hours, with a portion given in the initial hours after injury and the remainder given over the remaining hours.
A. Sterile dressing changes (option A) are incorrect because they are important in wound care management for burn patients to prevent infection. However, fluid resuscitation takes precedence within the first 24 hours.
B. Emotional support (option B) is incorrect because it is an essential aspect of burn care, as burn injuries can have a significant psychological impact. While emotional support is crucial for the patient's overall well-being, it may not be the highest priority within the first 24 hours compared to addressing the physiological needs of fluid resuscitation.
D. Range-of-motion exercises (option D) are incorrect because they are important for preventing contractures and maintaining joint mobility in burn patients. However, they are typically initiated after the initial fluid resuscitation phase and wound stabilization.
Therefore, the priority the nurse anticipates within the first 24 hours for a 31-year-old male patient with burn injuries is fluid resuscitation.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
A. Oxygen saturation of 92% in (option A) is incorrect because While an oxygen saturation of 92% is suboptimal and may require intervention, it may not have the same immediate implications as low blood pressure. The healthcare provider should be informed, but addressing the blood pressure takes priority.
B. Skin cool and clammy in (option B) is correct because Cool and clammy skin is often associated with inadequate peripheral perfusion, which is a characteristic of septic shock.
C. Septic shock is characterized by systemic inflammation, vasodilation, and hypotension. Inadequate blood pressure is a significant concern in septic shock as it indicates poor tissue perfusion and compromised organ function. However, the mean arterial pressure is till acceptable.
D. Heart rate of 118 beats/minute in (option D) is incorrect because: Tachycardia is a common finding in septic shock and reflects the body's compensatory response to maintain cardiac output. While it is a significant finding, low blood pressure takes precedence in terms of urgency.
Correct Answer is C
Explanation
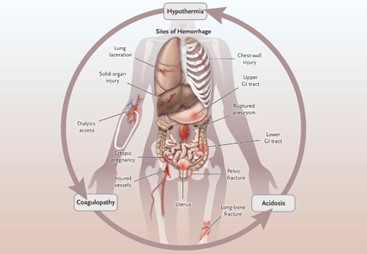
Hemorrhagic shock is characterized by severe blood loss, leading to inadequate tissue perfusion and hypovolemia. The primary goal in the initial management of hemorrhagic shock is to restore intravascular volume and improve tissue perfusion. Administering intravenous fluids, such as normal saline solution, is a critical intervention to address hypovolemia and improve blood pressure.
A. Give Plasmanate 1 unit now in (option A) is incorrect because: Plasmanate is a plasma-derived product used to replace coagulation factors. While it may be necessary to address coagulation abnormalities, administering intravenous fluids to restore volume takes priority over specific blood products.
B. Prepare for endotracheal intubation in (option B) is incorrect because Endotracheal intubation may be required in cases of impending respiratory failure or compromised airway, but it should not be the first action in addressing hypovolemic shock.
D. Type and crossmatch for 4 units of packed red blood cells (PRBCs) in (option D) is incorrect because transferring packed red blood cells is an important intervention to address blood loss and improve oxygen-carrying capacity. However, before administering blood products, it is crucial to stabilize the patient's hemodynamics through fluid resuscitation.
Therefore, in a patient with hemorrhagic shock, the nurse's first priority among the given options is to give normal saline solution of 250 mL/hr to restore intravascular volume and improve tissue perfusion.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
