Which of the following clinical manifestations is NOT considered part of Beck's triad (classic indications of cardiac tamponade)?
muffled heart tones
marked hypotension
distended jugular veins
widening pulse pressure
The Correct Answer is D
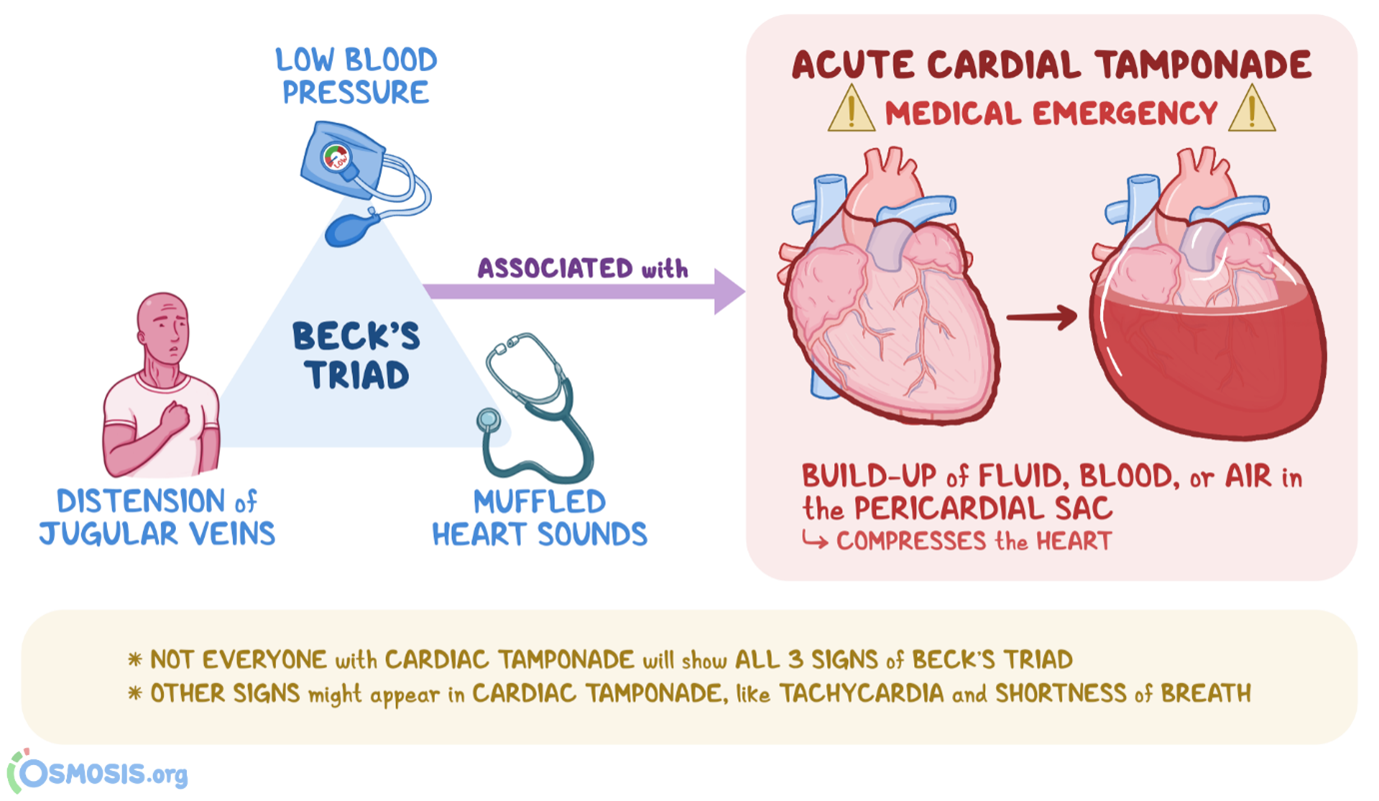
Beck's triad consists of three classic clinical manifestations that are suggestive of cardiac tamponade, which is the compression of the heart by accumulated fluid or blood within the pericardial sac. The three components of Beck's triad include:
A. Muffled heart tones in (option A) are incorrect because Cardiac tamponade can dampen or muffle heart sounds due to the presence of fluid or blood around the heart, which can impair sound transmission.
B. Marked hypotension in (option B) is incorrect because Cardiac tamponade can cause decreased cardiac output, leading to hypotension, which is characterized by low blood pressure.
C. Distended jugular veins in (option C) is incorrect because Elevated venous pressure resulting from impaired filling and elevated right-sided heart pressures can lead to jugular vein distension, which is commonly seen in cardiac tamponade.
However, widening pulse pressure (the difference between systolic and diastolic blood pressure) is not typically part of Beck's triad. Widening pulse pressure is associated with her conditions such as aortic regurgitation, hyperthyroidism, or conditions involving increased stroke volume, rather than cardiac tamponade specifically.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["9"]
Explanation
-
Doseinmcg/min=2mcg/kg/min×60kg=120mcg/min
Convert this to mg/min since the concentration is in mg:
120mcg/min=0.12mg/min120 \text{ mcg/min} = 0.12 \text{ mg/min}120mcg/min=0.12mg/min
-
Determine the concentration of Dopamine:
- Total amount of Dopamine: 200 mg in 250 mL of saline
- Concentration:
Concentration=200mg250mL=0.8mg/mL\text{Concentration} = \frac{200 \text{ mg}}{250 \text{ mL}} = 0.8 \text{ mg/mL}Concentration=250mL200mg=0.8mg/mL
-
Calculate the pump rate in mL/min:
To find the rate in mL/min needed to deliver 0.12 mg/min:
Pumprate=Desireddose(mg/min)Concentration(mg/mL)\text{Pump rate} = \frac{\text{Desired dose (mg/min)}}{\text{Concentration (mg/mL)}}Pumprate=Concentration(mg/mL)Desireddose(mg/min)
Pumprate=0.12mg/min0.8mg/mL=0.15mL/min\text{Pump rate} = \frac{0.12 \text{ mg/min}}{0.8 \text{ mg/mL}} = 0.15 \text{ mL/min}Pumprate=0.8mg/mL0.12mg/min=0.15mL/min
-
Convert the pump rate to mL/hour:
Multiply by 60 to convert from mL/min to mL/hour:
Pumprate=0.15mL/min×60min/hour=9mL/hour\text{Pump rate} = 0.15 \text{ mL/min} \times 60 \text{ min/hour} = 9 \text{ mL/hour}Pumprate=0.15mL/min×60min/hour=9mL/hour
So, you should set the pump to deliver Dopamine at a rate of 9 mL/hour.
Correct Answer is A
Explanation
The characteristics described in the monitor strip analysis suggest ventricular tachycardia. The absence of a visible P wave and the wide and distorted QRS complex indicates that the electrical impulse is originating in the ventricles rather than the atria. The ventricular rate of 196 and regular R-R intervals further support the diagnosis of ventricular tachycardia.
B. Atrial fibrillation in (option B) is incorrect because it is characterized by irregularly irregular R-R intervals and the absence of discernible P waves. The QRS complex is typically narrow
C. Atrial tachycardia in (option C) is incorrect because it would have a rapid atrial rate with regular R-R intervals, and P waves may or may not be discernible. The QRS complex is typically narrow.
D. Ventricular fibrillation in (option D) is incorrect because it would present as a chaotic, rapid, and irregular electrical activity with no discernible P waves, QRS complexes, or regular R-R intervals. It is a life-threatening emergency that requires immediate defibrillation.
Therefore, based on the provided information, the nurse would interpret the patient's cardiac rhythm as ventricular tachycardia. However, it is important to note that an accurate interpretation should be made by a qualified healthcare professional, and the patient's clinical context should also be considered.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
