A student is caring for a patient who suffered massive blood loss after trauma. How does the student correlate the blood loss with the patient's mean arterial pressure (MAP)?
It causes vasoconstriction and increased MAP.
Lower blood volume lowers MAP.
It raises cardiac output and MAP.
There is no direct correlation to MAP.
The Correct Answer is B
Mean arterial pressure (MAP) is a measure of the average pressure within the arteries during one cardiac cycle. It represents the perfusion pressure that drives blood flow to organs and tissues. MAP is calculated using the formula:
MAP = Diastolic blood pressure + 1/3 (Systolic blood pressure - Diastolic blood pressure)
Blood loss, particularly in cases of significant hemorrhage, leads to a decrease in blood volume. When blood volume decreases, there is less circulating blood available to generate pressure within the arterial system. This reduction in blood volume results in decreased MAP.
Therefore, in the case of massive blood loss after trauma, the student can correlate it with a lower blood volume, which in turn leads to a lower MAP. The decrease in blood volume reduces the perfusion pressure, compromising organ and tissue perfusion
A. It causes vasoconstriction and increased MAP in (option A) is incorrect because: While vasoconstriction can occur as a compensatory mechanism to maintain blood pressure, it does not necessarily lead to an increased MAP in the context of significant blood loss.
C. It raises cardiac output and MAP in (option C) is incorrect because Blood loss typically leads to a reduction in cardiac output due to decreased blood volume. Therefore, it does not raise cardiac output and MAP.
D. There is no direct correlation to MAP in (option D) is incorrect because: There is indeed a direct correlation between blood loss and MAP. As blood volume decreases, MAP decreases as well.
Therefore, the correct correlation between blood loss and MAP is that lower blood volume lowers MAP.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Tachypnoea, which refers to an increased respiratory rate, is an early symptom of hypovolemic shock. It is the body's compensatory response to inadequate tissue perfusion and decreased oxygen delivery. The increased respiratory rate is an attempt to improve oxygenation and maintain vital organ function.
B. Heart blocks in (option B) are incorrect because Heart blocks refer to disruptions in the electrical conduction system of the heart and are not specific to hypovolemic shock.
C. Vomiting in (option C) is incorrect because: Vomiting may occur in various conditions, including shock, but it is not exclusive to hypovolemic shock and can be present in other forms of shock or illnesses.
D. Bradycardia in (option D) is incorrect because Bradycardia, or a slow heart rate, is not typically an early symptom of hypovolemic shock. Instead, tachycardia (rapid heart rate) is more commonly observed as a compensatory response to maintain cardiac output.
E. Hypotension in (option E) is incorrect because Hypotension, or low blood pressure, can occur in hypovolemic shock but is generally considered a later-stage symptom. In the early stages, compensatory mechanisms may help maintain blood pressure, so hypotension may not be present initially.
F. Bradypnea in (option F) is incorrect because: Bradypnea refers to a slow respiratory rate, which is not typically an early symptom of hypovolemic shock. Tachypnoea, as mentioned earlier, is the more common early respiratory symptom.
Correct Answer is B
Explanation
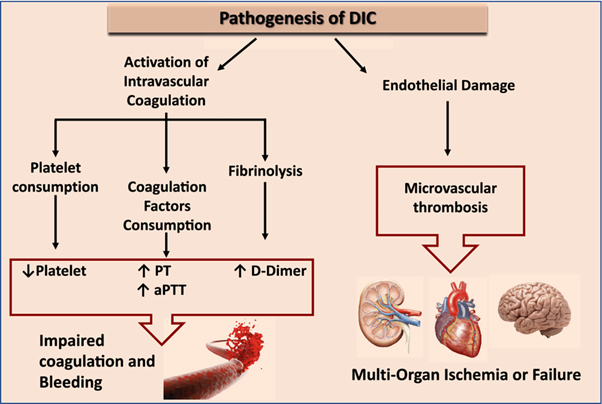
Disseminated Intravascular Coagulation (DIC) is a condition characterized by widespread activation of the coagulation system, leading to both excessive clot formation and consumption of clotting factors and platelets. This process can result in both bleeding and thrombosis.
The manifestations mentioned in option B are commonly seen in DIC:
Decreased platelet counts: DIC leads to platelet consumption and destruction, resulting in low platelet counts (thrombocytopenia).
Increased D-dimer: D-dimer is a fibrin degradation product, and its levels are increased DIC due to the breakdown of fibrin clots.
Increased prothrombin time (PT): DIC can lead to the depletion of clotting factors, resulting in prolonged prothrombin time, indicating impaired coagulation.
The other options mentioned do not represent the typical clinical manifestations of DIC:
A. Decreased hematocrit, increased platelet counts, and increased D-dimer in (option A) are incorrect because While platelet counts and D-dimer are increased in DIC, decreased hematocrit is not a characteristic finding.
C. Decreased Antithrombin III, increased platelet counts, and increased fibrinogen in (option C) is incorrect because: Decreased Antithrombin III can be seen in DIC, but increased platelet counts and fibrinogen levels are not specific to DIC.
D. Decreased D-dimer, increased platelet counts, and increased hemoglobin in (option D) is incorrect because Decreased D-dimer and increased hemoglobin are not typical findings in DIC, while increased platelet counts can be seen in some cases.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
