A 50-year-old male patient presents with facial rounding, central obesity, and purple striae on the abdomen. Laboratory results show high levels of ACTH. What is the most likely underlying cause of his condition?
Adrenal insufficiency.
Pheochromocytoma.
Cushing Disease.
Hyperthyroidism.
The Correct Answer is C
Choice A Reason:
Adrenal insufficiency, also known as Addison’s disease, is characterized by insufficient production of cortisol and aldosterone by the adrenal glands. Symptoms typically include fatigue, weight loss, low blood pressure, and hyperpigmentation of the skin. High levels of ACTH are not associated with adrenal insufficiency; instead, ACTH levels are usually elevated in response to low cortisol levels.
Choice B Reason:
Pheochromocytoma is a rare tumor of the adrenal gland that produces excess catecholamines, leading to symptoms such as hypertension, palpitations, and headaches. It does not cause high levels of ACTH or the physical manifestations described in the patient, such as facial rounding and purple striae.
Choice C Reason:
Cushing Disease is caused by a pituitary adenoma that secretes excess adrenocorticotropic hormone (ACTH), leading to overproduction of cortisol by the adrenal glands. This results in symptoms such as facial rounding (moon face), central obesity, purple striae on the abdomen, and high levels of ACTH. These clinical features align with the patient’s presentation, making Cushing Disease the most likely underlying cause.
Choice D Reason:
Hyperthyroidism is characterized by excessive production of thyroid hormones, leading to symptoms such as weight loss, heat intolerance, palpitations, and tremors. It does not cause high levels of ACTH or the specific physical changes seen in Cushing Disease.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason:
Administering intravenous fluids is not the most appropriate initial action for managing hypopituitarism. While IV fluids may be necessary in cases of acute adrenal crisis or severe dehydration, they do not address the underlying hormone deficiencies caused by hypopituitarism. The primary treatment focuses on replacing the deficient hormones to restore normal physiological functions.
Choice B Reason:
Performing a transsphenoidal hypophysectomy is a surgical procedure used to remove pituitary tumors. While this may be necessary if a tumor is causing hypopituitarism, it is not the initial action for managing the condition. The first step is to stabilize the patient with hormone replacement therapy before considering surgical interventions.
Choice C Reason:
Initiating hormone replacement therapy is the most appropriate initial action for managing hypopituitarism. This condition results in the deficiency of one or more pituitary hormones, and replacing these hormones is crucial to restore normal body functions. Hormone replacement therapy may include cortisol, thyroid hormone, sex hormones, and growth hormone, depending on which hormones are deficient.
Choice D Reason:
Recommending dietary modifications alone is not sufficient to manage hypopituitarism. While a balanced diet can support overall health, it does not address the specific hormone deficiencies associated with this condition. Hormone replacement therapy is essential for managing hypopituitarism effectively.
Correct Answer is B
Explanation
Choice A: Instruct the patient to elevate the arm above the heart immediately after the procedure
Elevating the arm above the heart can help reduce blood flow to the area, potentially minimizing bleeding. However, this method alone is not sufficient to ensure proper hemostasis, especially in patients with thrombocytopenia. Applying direct pressure to the puncture site is more effective in stopping bleeding and preventing hematoma formation.
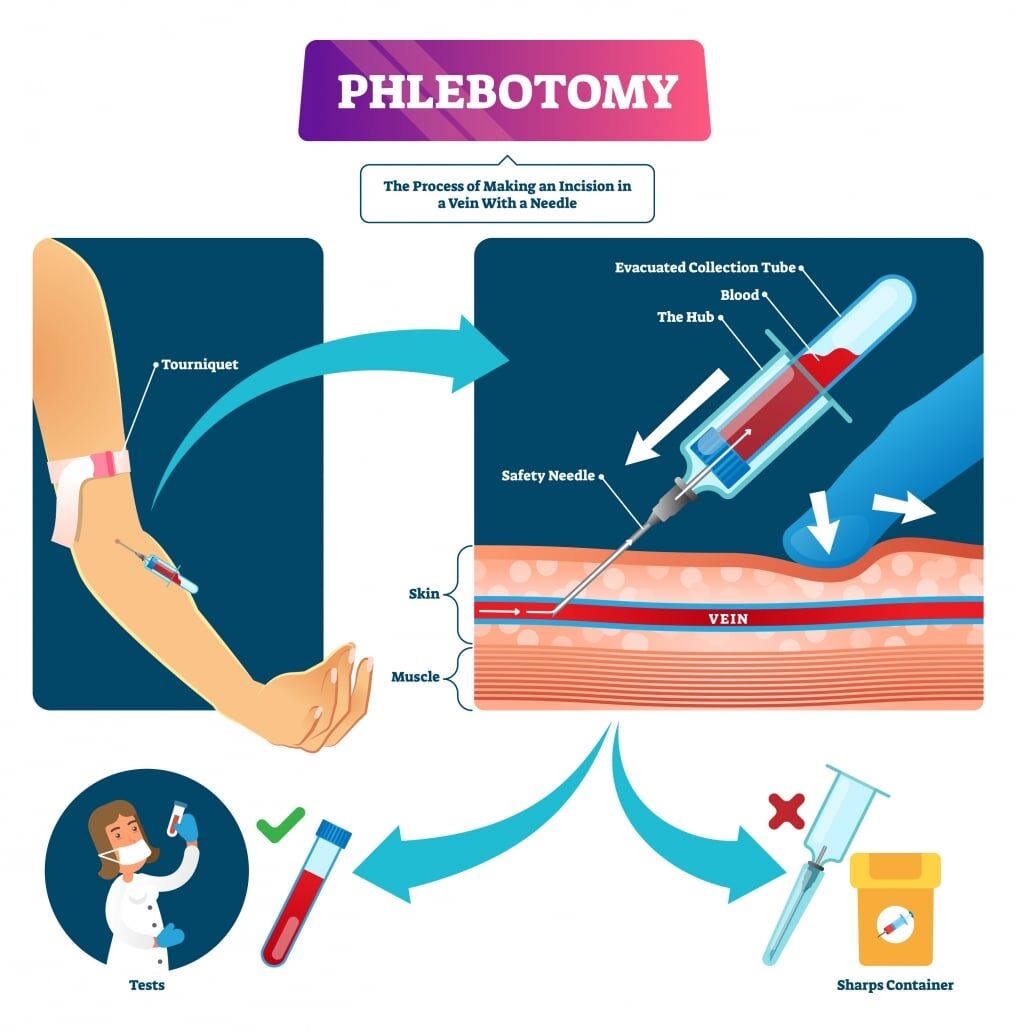
Choice B: Apply firm pressure to the site for at least 10 minutes after the procedure
Applying firm pressure to the venipuncture site is crucial in patients with thrombocytopenia to ensure proper clotting and prevent bleeding. This method helps in forming a stable clot at the puncture site, reducing the risk of prolonged bleeding and hematoma formation. Given the patient’s low platelet count, maintaining pressure for an extended period is essential to achieve hemostasis.
Choice C: Avoid using a tourniquet during the procedure
While avoiding a tourniquet might seem beneficial to reduce pressure on the veins, it is not a standard practice to minimize bleeding risk in thrombocytopenic patients. Tourniquets are typically used to make veins more prominent for easier access during venipuncture. The key to minimizing bleeding is proper post-procedure care, such as applying firm pressure to the site.
Choice D: Use a larger gauge needle to ensure quicker blood flow
Using a larger gauge needle is not advisable for patients with thrombocytopenia. Larger needles can cause more trauma to the vein, increasing the risk of bleeding and hematoma formation. Instead, using the smallest gauge needle that can effectively draw blood is recommended to minimize vein damage.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
