A 55-year-old patient with type 2 diabetes is admitted to the hospital and is on NPH insulin. The patient experiences symptoms of hypoglycemia. At what time after administration of NPH insulin should the nurse be most vigilant for signs of hypoglycemia due to the peak action of the insulin?
18-24 hours after administration
4-12 hours after administration
12-18 hours after administration
1-2 hours after administration
The Correct Answer is B
Choice A Reason:
NPH insulin is an intermediate-acting insulin that typically has a duration of action of about 12 to 16 hours. The peak action, however, occurs much earlier, making 18-24 hours after administration an incorrect choice for the peak time of hypoglycemia risk.
Choice B Reason:
NPH insulin generally peaks 4 to 12 hours after administration This is the period when the insulin is most effective at lowering blood glucose levels, and therefore, the time when the patient is at the highest risk for hypoglycemia. Monitoring for signs of hypoglycemia during this window is crucial to ensure patient safety.
Choice C Reason:
While NPH insulin can have effects lasting up to 16 hours, the peak action occurs earlier, between 4 to 12 hours. Therefore, 12-18 hours after administration is not the correct time frame for the peak action of NPH insulin.
Choice D Reason:
NPH insulin starts to act within 1 to 2 hours after administration, but this is not the peak time. The peak action, when the risk of hypoglycemia is highest, occurs later, between 4 to 12 hours after administration.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
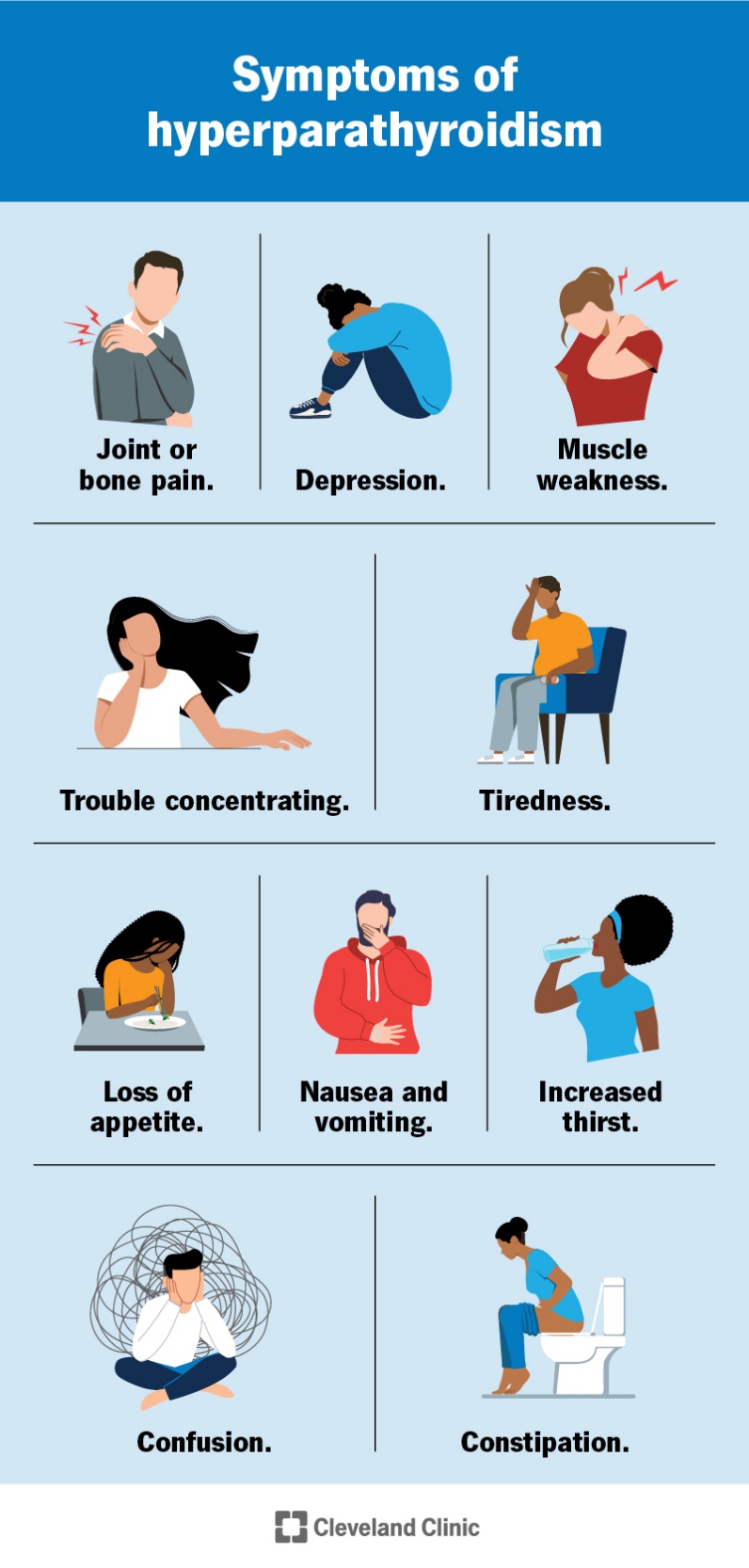
Choice A Reason:
An adenoma of the parathyroid gland is the most common cause of primary hyperparathyroidism. This benign tumor leads to the overproduction of parathyroid hormone (PTH), which in turn causes elevated calcium levels in the blood. The excessive PTH secretion disrupts the normal calcium balance, leading to symptoms such as fatigue, muscle weakness, and depression. Parathyroid adenomas account for approximately 80% of primary hyperparathyroidism cases.
Choice B Reason:
Thyroid carcinoma is a type of cancer that originates in the thyroid gland, not the parathyroid glands. While thyroid carcinoma can cause various symptoms, it does not typically lead to elevated PTH levels or hyperparathyroidism. Therefore, it is not the most likely cause of the patient’s condition.
Choice C Reason:
Vitamin D deficiency can lead to secondary hyperparathyroidism, where low levels of vitamin D cause decreased calcium absorption, prompting the parathyroid glands to produce more PTH to maintain calcium levels. However, this condition is usually associated with low or normal calcium levels, not elevated calcium levels as seen in this patient. Therefore, it is not the most likely cause of her hyperparathyroidism.
Choice D Reason:
Chronic kidney disease (CKD) can also cause secondary hyperparathyroidism due to impaired kidney function, which affects calcium and phosphate balance and vitamin D metabolism. However, similar to vitamin D deficiency, CKD-related hyperparathyroidism typically presents with low or normal calcium levels rather than elevated levels. Thus, it is not the most likely cause in this scenario.
Correct Answer is C
Explanation
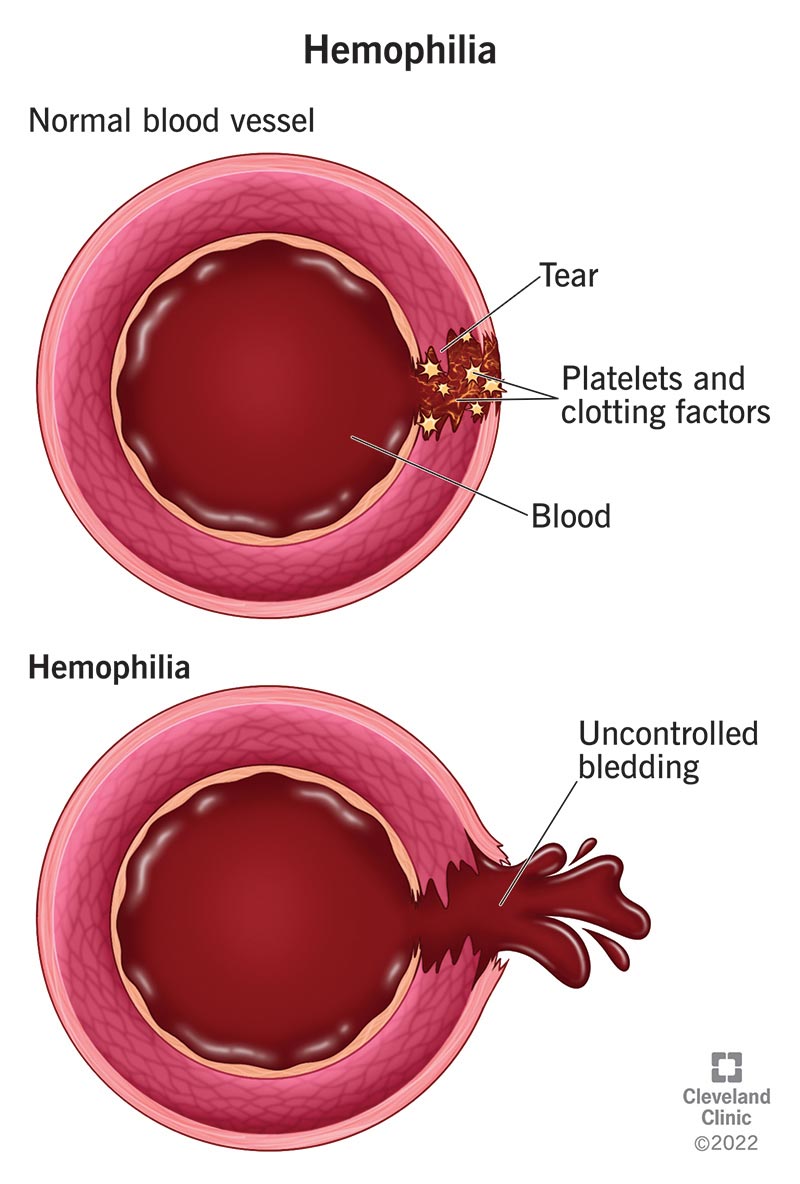
Choice A Reason:
Preparing the patient for immediate surgical intervention is not the first-line treatment for hemophilia-related joint bleeding. Surgery is considered only if there is severe damage or if conservative measures fail. Initial management focuses on controlling bleeding and reducing inflammation.
Choice B Reason:
Administering aspirin for pain relief is contraindicated in patients with hemophilia. Aspirin inhibits platelet function and can exacerbate bleeding. Alternative pain management strategies that do not affect clotting should be used.
Choice C Reason:
Applying ice to the affected knee and elevating the leg is the most appropriate initial intervention. Ice helps to reduce swelling and pain, while elevation minimizes blood flow to the area, helping to control bleeding. This conservative approach is crucial in managing acute hemarthrosis in hemophilia patients.
Choice D Reason:
Performing passive range of motion exercises on the affected knee is not recommended during the acute phase of hemarthrosis. Movement can increase bleeding and worsen the condition. Rest and immobilization are preferred until the bleeding is controlled.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
