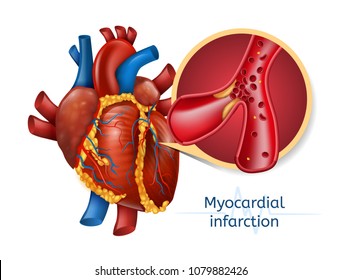
A 52-year-old male suffered a myocardial infarction secondary to atherosclerosis and ischemia. Once oxygen returned to the damaged heart, reperfusion injury occurred as a result of:
Oxygenation of the cells
Free radical formation
Increased metabolic state
Lactic acid build-up
The Correct Answer is B
Choice A Reason:
Oxygenation of the cells is a necessary process during reperfusion, but it is not the direct cause of reperfusion injury. The injury occurs due to the sudden influx of oxygen, which leads to the formation of reactive oxygen species (ROS) or free radicals. These free radicals cause oxidative stress and damage to the myocardial cells.
Choice B Reason:
Free radical formation is the primary mechanism behind reperfusion injury. When blood flow is restored to the ischemic myocardium, the sudden reintroduction of oxygen leads to the production of free radicals. These free radicals cause significant oxidative damage to the cell membranes, proteins, and DNA, exacerbating the injury to the heart tissue.
Choice C Reason:
An increased metabolic state can occur during reperfusion as the cells attempt to recover from ischemia. However, it is not the direct cause of reperfusion injury. The primary issue is the oxidative stress caused by free radicals, not the metabolic changes themselves.
Choice D Reason:
Lactic acid build-up is a consequence of anaerobic metabolism during the ischemic period, not a cause of reperfusion injury. During ischemia, cells switch to anaerobic metabolism, leading to lactic acid accumulation. However, once oxygen is reintroduced, the focus shifts to the oxidative damage caused by free radicals rather than lactic acid.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
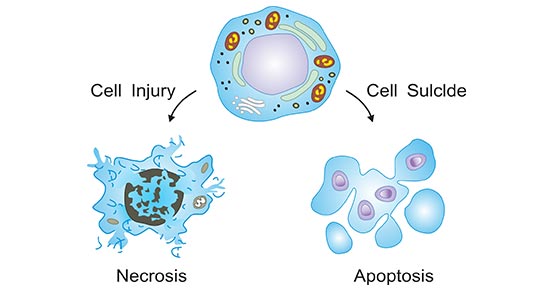
Choice A: Atrophy
Atrophy refers to the reduction in size or wasting away of an organ or tissue due to a decrease in cell size or number. This can occur due to various reasons such as disuse, lack of nutrition, or loss of nerve supply. While atrophy involves the shrinkage of cells, it does not directly result in cellular death. Instead, it is a form of cellular adaptation to adverse conditions.
Choice B: Proliferation
Proliferation is the process by which cells grow and divide to produce more cells. This process is essential for growth, development, and tissue repair. Proliferation leads to an increase in the number of cells and is the opposite of cellular death. It is a tightly regulated process that ensures the maintenance and regeneration of tissues.
Choice C: Mutation
Mutation refers to changes in the DNA sequence of a cell. These changes can occur due to errors during DNA replication, exposure to radiation, or chemical mutagens. While mutations can lead to various outcomes, including cancer, they do not directly cause cellular death. Instead, mutations can alter the function of genes and proteins, potentially leading to uncontrolled cell growth or other cellular dysfunctions.
Choice D: Death
Apoptosis is a form of programmed cell death that occurs in multicellular organisms. It is a highly regulated process that allows the body to remove damaged or unnecessary cells without causing harm to surrounding tissues. Apoptosis involves a series of biochemical events leading to characteristic cell changes and eventual death. This process is crucial for maintaining cellular homeostasis and preventing the development of diseases such as cancer.
Correct Answer is B
Explanation
Choice A Reason:
Vomiting is not a risk factor for a heart attack but rather a symptom that can occur during a heart attack. Risk factors are conditions or behaviors that increase the likelihood of developing a disease. Vomiting can be a sign of various conditions, including gastrointestinal issues or even a heart attack, but it does not contribute to the risk of having a heart attack.
Choice B Reason:
Hypertension, or high blood pressure, is a significant risk factor for heart attacks. It causes the heart to work harder than normal, leading to the thickening of the heart muscle and narrowing of the arteries. Over time, this increased workload can damage the arteries, making them more susceptible to blockages that can cause a heart attack. Managing blood pressure through lifestyle changes and medication is crucial in reducing the risk of heart attacks.
Choice C Reason:
Chest pain is a common symptom of a heart attack but not a risk factor. Risk factors are pre-existing conditions or behaviors that increase the likelihood of developing a disease. Chest pain, also known as angina, occurs when there is reduced blood flow to the heart muscle, often due to blockages in the coronary arteries. While chest pain indicates a potential heart problem, it is not a contributing factor to the development of a heart attack.
Choice D Reason:
Cell necrosis refers to the death of cells, which can occur during a heart attack when the blood supply to part of the heart muscle is blocked. This is a consequence of a heart attack rather than a risk factor. Risk factors are conditions or behaviors that increase the likelihood of developing a disease, whereas cell necrosis is a result of the disease process.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
