A 55-year-old patient with thrombocytopenia is scheduled for a venipuncture procedure. Which of the following actions should the nurse take to minimize the risk of bleeding?
Instruct the patient to elevate the arm above the heart immediately after the procedure.
Apply firm pressure to the site for at least 10 minutes after the procedure.
Avoid using a tourniquet during the procedure.
Use a larger gauge needle to ensure quicker blood flow.
The Correct Answer is B
Choice A: Instruct the patient to elevate the arm above the heart immediately after the procedure
Elevating the arm above the heart can help reduce blood flow to the area, potentially minimizing bleeding. However, this method alone is not sufficient to ensure proper hemostasis, especially in patients with thrombocytopenia. Applying direct pressure to the puncture site is more effective in stopping bleeding and preventing hematoma formation.
Choice B: Apply firm pressure to the site for at least 10 minutes after the procedure
Applying firm pressure to the venipuncture site is crucial in patients with thrombocytopenia to ensure proper clotting and prevent bleeding. This method helps in forming a stable clot at the puncture site, reducing the risk of prolonged bleeding and hematoma formation. Given the patient’s low platelet count, maintaining pressure for an extended period is essential to achieve hemostasis.
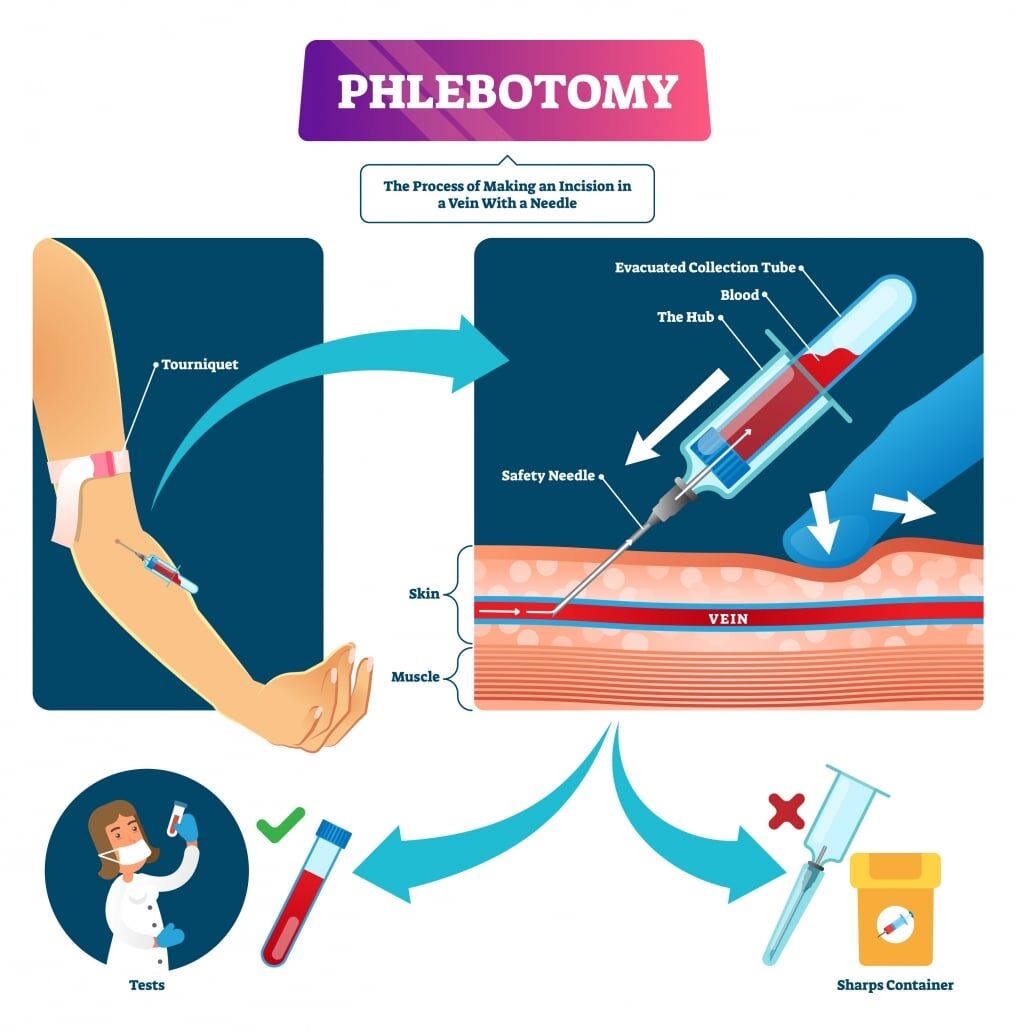
Choice C: Avoid using a tourniquet during the procedure
While avoiding a tourniquet might seem beneficial to reduce pressure on the veins, it is not a standard practice to minimize bleeding risk in thrombocytopenic patients. Tourniquets are typically used to make veins more prominent for easier access during venipuncture. The key to minimizing bleeding is proper post-procedure care, such as applying firm pressure to the site.
Choice D: Use a larger gauge needle to ensure quicker blood flow
Using a larger gauge needle is not advisable for patients with thrombocytopenia. Larger needles can cause more trauma to the vein, increasing the risk of bleeding and hematoma formation. Instead, using the smallest gauge needle that can effectively draw blood is recommended to minimize vein damage.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A Reason:
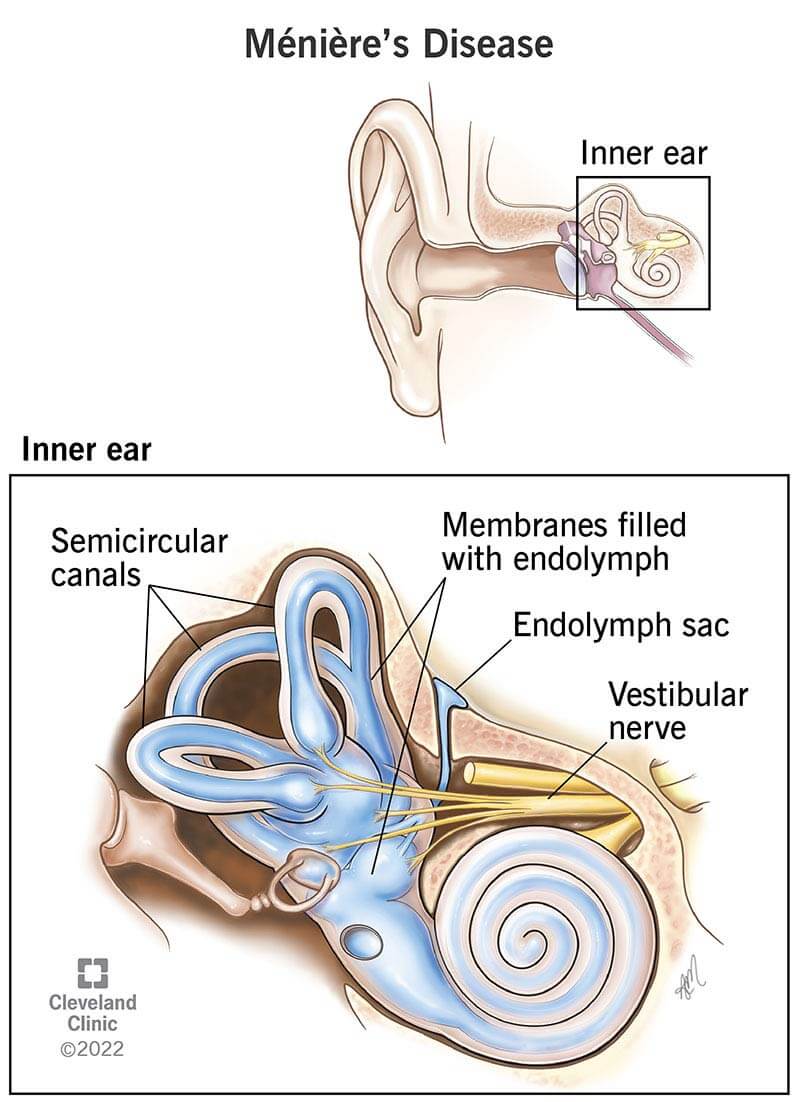
Caffeine-rich beverages are not recommended for patients with Meniere’s disease. Caffeine can exacerbate symptoms such as vertigo and tinnitus by increasing the fluid pressure in the inner ear. Therefore, avoiding caffeine is generally advised to help manage the condition.
Choice B Reason:
A low-sodium diet is an appropriate treatment for Meniere’s disease. Reducing sodium intake helps decrease fluid retention in the body, including the inner ear, which can alleviate symptoms such as vertigo, tinnitus, and hearing loss. This dietary modification is a cornerstone of managing Meniere’s disease and can significantly improve the patient’s quality of life.
Choice C Reason:
High-intensity interval training (HIIT) is not suitable for patients with Meniere’s disease. Intense physical activity can trigger vertigo attacks and worsen balance issues. Patients are generally advised to engage in moderate, low-impact exercises that do not provoke symptoms.
Choice D Reason:
Prolonged bed rest is not an appropriate treatment for Meniere’s disease. While rest may be necessary during acute vertigo attacks, long-term bed rest can lead to deconditioning and other health issues. It is important for patients to maintain a balance between rest and activity to manage their symptoms effectively.
Correct Answer is ["B","C","D","F"]
Explanation
Choice A Reason:
Acetone breath is typically associated with diabetic ketoacidosis (DKA), not hyperosmolar hyperglycemic syndrome (HHS). DKA occurs when there is a significant production of ketones due to the breakdown of fat for energy, leading to a fruity or acetone-like smell on the breath. HHS, on the other hand, does not usually involve significant ketone production.
Choice B Reason:
Fever can be a manifestation of HHS, especially if there is an underlying infection or illness that has precipitated the hyperglycemic crisis. Infections are common triggers for HHS and can contribute to the severity of the condition.
Choice C Reason:
Older age is a risk factor for HHS. HHS is more commonly seen in older adults with type 2 diabetes, often those who have underlying chronic conditions or are experiencing acute illness. The patient’s age of 68 years supports the likelihood of HHS.
Choice D Reason:
A serum glucose level of 800 mg/dL is indicative of HHS. HHS is characterized by extremely high blood glucose levels, often exceeding 600 mg/dL, without significant ketone production. This high glucose level leads to severe dehydration and hyperosmolarity.
Choice E Reason:
A serum bicarbonate level of 15 mEq/L is more indicative of DKA rather than HHS. In HHS, serum bicarbonate levels are typically normal or only mildly decreased because there is no significant ketoacidosis. Therefore, this choice does not support the clinical presentation of HHS.
Choice F Reason:
An insidious onset is characteristic of HHS. Unlike DKA, which can develop rapidly, HHS often develops over days to weeks. Patients may experience gradually worsening symptoms such as increased thirst, frequent urination, and confusion before seeking medical attention.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
