A client comes to the clinic for an evaluation. The client is at 22 weeks' gestation. After reviewing a client's history, which factor would the nurse identify as placing her at risk for preeclampsia?
Client has a twin sister.
Her mother had preeclampsia during pregnancy.
This is the client's second pregnancy.
Her sister-in-law had gestational hypertension.
The Correct Answer is B
A. Client has a twin sister.
Having a twin sister does not directly increase the client's risk of developing preeclampsia. While twin pregnancies are associated with higher rates of certain complications, such as preterm birth and gestational hypertension, having a twin sister herself does not inherently increase her risk of preeclampsia.
B. Her mother had preeclampsia during pregnancy.
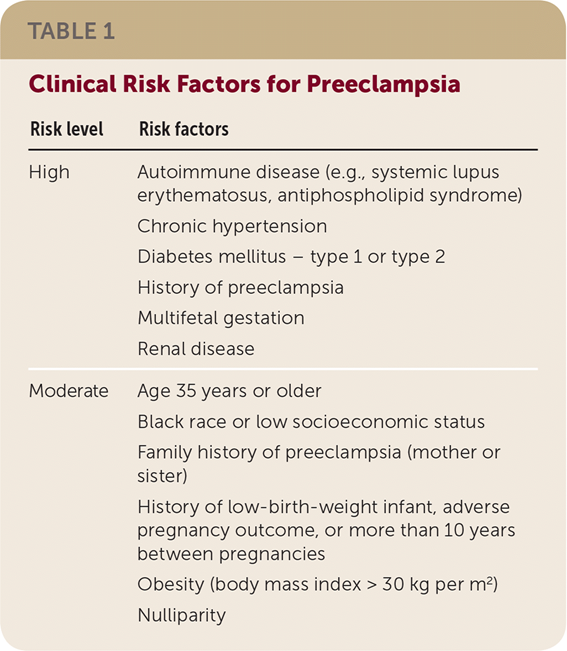
This is the correct choice. A history of preeclampsia in the client's mother is a significant risk factor for preeclampsia in the client herself. Preeclampsia has a genetic component, and women with a family history of the condition, especially in their mothers, are at increased risk of developing it during their own pregnancies.
C. This is the client's second pregnancy.
While the number of pregnancies a woman has experienced can influence her risk of certain pregnancy complications, such as placental abnormalities, it is not as strong a risk factor for preeclampsia as a family history of the condition. Preeclampsia can occur in both first and subsequent pregnancies, regardless of the number of pregnancies a woman has had.
D. Her sister-in-law had gestational hypertension.
Gestational hypertension is a related condition to preeclampsia and shares some risk factors, such as high blood pressure during pregnancy. However, a sister-in-law having gestational hypertension does not directly increase the client's risk of preeclampsia. While it may suggest a family predisposition to hypertensive disorders during pregnancy, it is not as specific a risk factor for preeclampsia as a direct family history of the condition, such as in the client's mother.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
A. "I'm sorry you lost your baby."
This response demonstrates empathy and validation of the client's emotions. It acknowledges the client's loss and offers support during a difficult time. By expressing sympathy, the nurse shows understanding and compassion towards the client's grief.
B. "A baby still wasn't formed in your uterus."
This response may come across as dismissive or invalidating of the client's emotions. It does not acknowledge the client's loss or address their emotional needs. It focuses more on the biological aspect of the situation rather than the client's feelings.
C. "Will a pill help your pain?"
This response only addresses physical pain management and does not acknowledge the emotional distress the client is experiencing. While pain relief is important, it is equally important to address the client's emotional needs and provide support during a difficult time.
D. "Why are you crying?"
This response may come across as insensitive or intrusive. It puts the client on the spot and may make them feel uncomfortable or defensive about their emotions. It does not provide empathy or support and fails to acknowledge the client's loss or offer condolences.
Correct Answer is ["A","C","E"]
Explanation
A. Engaging in daily exercise:
Regular physical activity has been associated with a reduced risk of endometrial cancer. Exercise helps maintain a healthy weight and may help regulate hormone levels, which can contribute to a lower risk of developing endometrial cancer.
B. Eating a high-fat diet:
Consuming a high-fat diet may increase the risk of endometrial cancer. High-fat diets have been linked to obesity, which in turn is a risk factor for endometrial cancer. Additionally, high-fat diets may alter hormone levels in the body, potentially affecting the development of endometrial cancer.
C. Becoming pregnant:
Pregnancy and childbirth can have a protective effect against endometrial cancer. During pregnancy, hormonal changes and the cessation of menstrual cycles may reduce the exposure of the endometrium to estrogen, potentially decreasing the risk of developing endometrial cancer.
D. Using estrogen contraceptives:
Estrogen-containing contraceptives, such as birth control pills, patches, or hormonal intrauterine devices (IUDs), have been associated with a higher risk of endometrial cancer, especially if used for extended periods. Estrogen alone, without the balancing effect of progesterone, can stimulate the growth of the endometrium and increase the risk of cancer.
E. Having regular pelvic exams:
Regular pelvic exams, which may include a Pap smear and/or endometrial biopsy, can help detect abnormalities in the endometrium at an early stage. Early detection can lead to timely intervention and treatment, potentially reducing the risk of advanced endometrial cancer.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
