A neonate born to a mother who was abusing heroin is exhibiting signs and symptoms of withdrawal. Which signs would the nurse assess? (Select All that Apply.)
hypertonicity
excessive sneezing
low whimpering cry
overly vigorous sucking
lethargy
tremors
Correct Answer : A,B,C,D,E,F
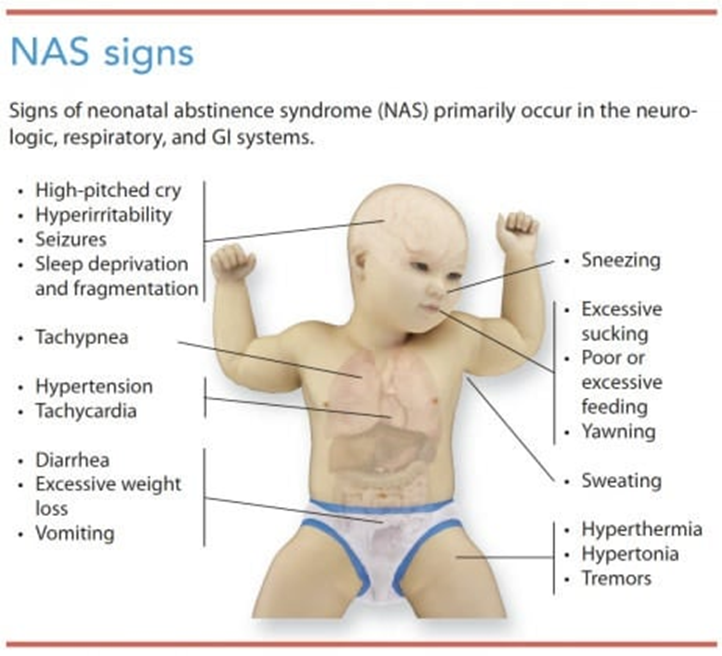
A. Hypertonicity: Neonates experiencing withdrawal from heroin may exhibit increased muscle tone, leading to stiffness or rigidity. This is often observed as hypertonicity in their limbs or overall body.
B. Excessive sneezing: Nasal congestion and sneezing are common symptoms in neonates undergoing withdrawal. These symptoms can occur due to the irritant effects of withdrawal on the respiratory system.
C. Low whimpering cry: Infants with neonatal abstinence syndrome (NAS) may have a weak or high-pitched cry, which may sound like whimpering. This cry can be indicative of the discomfort and distress they are experiencing.
D. Overly vigorous sucking: Neonates with NAS may display exaggerated sucking behaviors, often characterized by frantic or overly vigorous sucking during feeding or when provided with a pacifier. This behavior is a manifestation of their heightened agitation and irritability.
E. Lethargy: Some neonates experiencing NAS may appear excessively drowsy, fatigued, or have decreased responsiveness. Lethargy is a common symptom associated with withdrawal from heroin or other opioids.
F. Tremors: Tremors or shaking movements, especially when the neonate is disturbed or agitated, are hallmark signs of NAS. These tremors can be mild to severe and may affect various parts of the body, such as the arms, legs, or jaw.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
A. 24 hours before birth and 24 hours after birth:
This option suggests administering Rho(D) immune globulin (RhIg) both before and after birth. However, the standard recommendation is to administer RhIg at 28 weeks' gestation and again within 72 hours after birth. Administering RhIg before birth in this manner is not a standard practice for preventing Rh isoimmunization.
B. At 28 weeks' gestation and again within 72 hours after birth:
This is the correct choice. Administering RhIg at 28 weeks' gestation helps prevent sensitization of the Rh-negative mother to Rh-positive fetal blood cells that may have entered her circulation during pregnancy. Administering it again within 72 hours after birth helps prevent sensitization from any Rh-positive fetal blood cells that may have entered the mother's circulation during delivery.
C. At 32 weeks' gestation and immediately before discharge:
Administering RhIg at 32 weeks' gestation is not the standard recommendation. The standard timing is at 28 weeks' gestation to cover the critical period of sensitization during pregnancy. Administering it immediately before discharge may not provide adequate protection if sensitization has already occurred during pregnancy.
D. In the first trimester and within 2 hours of birth:
Administering RhIg in the first trimester is not a routine practice unless there is a specific indication, such as miscarriage or invasive procedures that may lead to fetal-maternal hemorrhage. Administering it within 2 hours of birth alone does not provide adequate protection against sensitization during pregnancy. The standard recommendation is to administer RhIg at 28 weeks' gestation and again within 72 hours after birth to cover the critical periods of sensitization during pregnancy and delivery.
Correct Answer is D
Explanation
A. Immunization:
Currently, there is no licensed vaccine available for the prevention of cytomegalovirus (CMV) infection. Therefore, immunization is not a viable option for preventing CMV infection during pregnancy. While researchers are actively working on developing a CMV vaccine, it is not yet available for widespread use.
B. Prenatal screening:
Prenatal screening for CMV is not routinely performed during prenatal care. Screening for CMV during pregnancy is not typically recommended unless there is a specific clinical indication, such as maternal symptoms suggestive of acute CMV infection or fetal abnormalities detected on ultrasound. Therefore, prenatal screening is not a primary preventive measure for CMV infection during pregnancy.
C. Antibody titer screening:
Antibody titer screening for CMV is also not routinely performed during prenatal care. While some healthcare providers may offer CMV antibody testing in certain situations, such as for women with a known exposure to CMV or those at increased risk of primary CMV infection during pregnancy, it is not a standard practice for all pregnant women. Therefore, antibody titer screening is not a primary preventive measure for CMV infection during pregnancy.
D. Frequent handwashing:
Frequent handwashing is the most important preventive measure for reducing the risk of CMV infection during pregnancy. CMV is commonly transmitted through close contact with bodily fluids, such as saliva, urine, blood, and genital secretions. Proper hand hygiene, including washing hands with soap and water for at least 20 seconds, especially after coming into contact with young children's saliva or urine, can help prevent the spread of CMV. This measure is crucial for pregnant women to reduce their risk of acquiring CMV and transmitting it to their unborn babies.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
