A client with insulin-dependent type 2 diabetes and an HbA1c of 6.0% is planning to become pregnant soon. What anticipatory teaching should the nurse provide this client?
Select one:
Insulin needs decrease in the first trimester, but increase in the second trimester as the woman's body becomes more insulin-resistant.
Vascular disease that always accompanies diabetes slows fetal growth.
The risk of ketoacidosis decreases during the length of the pregnancy.
The baby is likely to have a congenital abnormality because of the uncontrolled diabetes.
The Correct Answer is A
Choice A Reason: Insulin needs decrease in the first trimester, but increase in the second trimester as the woman's body becomes more insulin-resistant. This is because this statement describes the typical patern of insulin requirements during pregnancy for women with pre-existing diabetes. Insulin needs decrease in the first trimester due to increased insulin production by the pancreas, increased insulin sensitivity by the tissues, and increased risk of hypoglycemia due to nausea and vomiting. Insulin needs increase in the second trimester due to increased levels of placental hormones such as human placental lactogen (hPL), which antagonize insulin action and cause insulin resistance.
Choice B Reason: Vascular disease that always accompanies diabetes slows fetal growth. This is an incorrect answer that makes a false and exaggerated claim about diabetes and fetal growth. Vascular disease does not always accompany diabetes, but it can be a complication of long-term or poorly controlled diabetes that affects blood vessels and circulation. Vascular disease can affect fetal growth by reducing placental perfusion and oxygen delivery, but it is not the only factor that influences fetal growth. Other factors include maternal nutrition, genetics, infections, or anomalies.
Choice C Reason: The risk of ketoacidosis decreases during the length of the pregnancy. This is an incorrect answer that contradicts the evidence and guidelines on diabetes and ketoacidosis during pregnancy. Ketoacidosis is a metabolic emergency where high levels of ketones accumulate in the blood due to insufficient insulin or excessive glucose utilization, which causes acidosis, dehydration, electrolyte imbalance, and coma. Ketoacidosis can occur in women with diabetes during pregnancy due to infection, stress, starvation, or inadequate insulin therapy. The risk of ketoacidosis does not decrease during the length of the pregnancy, but rather increases in the second and third trimesters due to increased insulin resistance and glucose production.
Choice D Reason: The baby is likely to have a congenital abnormality because of the uncontrolled diabetes. This is an incorrect answer that implies a negative and deterministic outcome for the baby. Congenital abnormalities are structural or functional defects that are present at birth, which can affect various organs or systems in the baby.
Congenital abnormalities can be caused by genetic or environmental factors, or a combination of both. Diabetes can increase the risk of congenital abnormalities, especially if the blood glucose levels are high during the first trimester, when organogenesis occurs. However, the risk of congenital abnormalities is not inevitable or predictable, and it can be reduced by maintaining good glycemic control before and during pregnancy.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
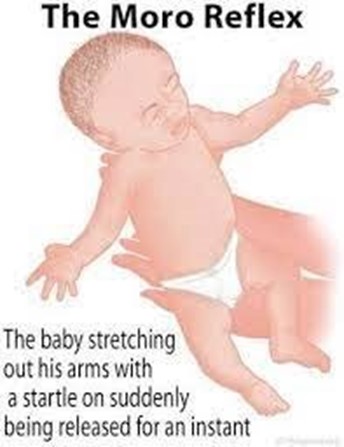
Choice A Reason: The cheek of the newborn is touched, and the newborn turns toward the side that was touched. This is an incorrect answer that describes a different reflex called the rooting reflex. The rooting reflex is a feeding reflex that helps the newborn locate the nipple and initiate sucking. The rooting reflex is elicited by stroking the cheek or corner of the mouth of the newborn, which causes them to turn their head and open their mouth toward the stimulus.
Choice B Reason: The newborn is suddenly lowered or startled, and they extend their arms, legs and neck, then rapidly bring their arms together. This is because this response describes the Moro reflex, which is a primitive reflex that is present at birth and disappears by 3 to 6 months of age. The Moro reflex is elicited by simulating a falling sensation or a loud noise, which triggers a fear response in the newborn. The Moro reflex consists of four phases: extension, abduction, adduction, and crying.
Choice C Reason: The newborn is supine and their head is turned to one side, then the arm on that same side extends. This is an incorrect answer that refers to another reflex called the tonic neck reflex. The tonic neck reflex is a postural reflex that helps prepare the newborn for voluntary reaching. The tonic neck reflex is elicited by placing the newborn in a supine position and turning their head to one side, which causes them to assume a "fencing" posture with one arm extended and one arm flexed.
Choice D Reason: The lateral aspect of the sole of the newborn's foot is stroked, and the toes extend and fan outward. This is an incorrect answer that indicates a different reflex called the Babinski reflex. The Babinski reflex is a neurological reflex that tests for spinal cord integrity. The Babinski reflex is elicited by stroking the lateral aspect of the sole of the foot from heel to toe, which causes the big toe to dorsiflex and the other toes to fan out.
Correct Answer is A
Explanation
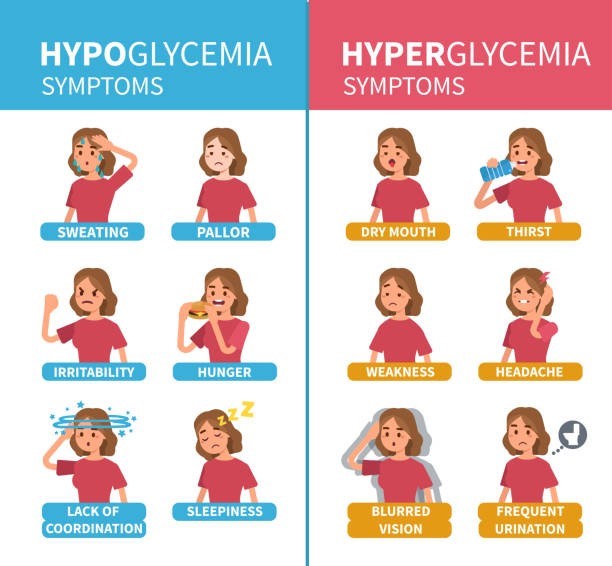
Choice A Reason: Episodes of hypoglycemia and hyperglycemia. This is because episodes of hypoglycemia and hyperglycemia are common complications of diabetes during pregnancy, which can affect both the mother and the fetus. Hypoglycemia is a condition where the blood glucose level drops below the normal range, which can cause symptoms such as sweating, trembling, hunger, confusion, or loss of consciousness. Hyperglycemia is a condition where the blood glucose level rises above the normal range, which can cause symptoms such as thirst, polyuria, fatigue, blurred vision, or ketoacidosis. Diabetes during pregnancy requires careful monitoring and management of blood glucose levels to prevent adverse outcomes such as fetal macrosomia, congenital anomalies, stillbirth, or neonatal hypoglycemia.
Choice B Reason: Postpartum hemorrhage. This is an incorrect answer that refers to a different complication that may occur after delivery, not during pregnancy. Postpartum hemorrhage is excessive bleeding from the uterus or genital tract after delivery, which can cause hypovolemic shock, anemia, or death. Postpartum hemorrhage can be caused by uterine atony, retained placenta, lacerations, or coagulation disorders.
Choice C Reason: Cerebrovascular accident (CVA). This is an incorrect answer that indicates a rare and severe complication that may occur during or after pregnancy, not specifically related to diabetes. CVA is also known as stroke, which is an interruption of blood flow to the brain due to ischemia or hemorrhage, which can cause neurological deficits or death. CVA can be caused by hypertension, preeclampsia-eclampsia, thrombophilia, or vascular malformations.
Choice D Reason: Acute vasospasm. This is an incorrect answer that suggests a different condition that may occur during pregnancy, not associated with diabetes. Acute vasospasm is also known as Raynaud's phenomenon, which is a disorder of blood vessels that causes them to narrow and reduce blood flow to the extremities in response to cold or stress, which can cause pain, numbness, or color changes. Acute vasospasm can be triggered by smoking, medications, or autoimmune diseases.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
