The patient is 34 weeks pregnant and during a regular prenatal visit she asks how to do kick counts. The best response by the nurse would be:
Select one:
Fetal movements are an indicator of fetal well-being. You should count twice a day, and you should feel ten fetal movements in 2 hours.
Here is a computer printed information packet on how to do kick counts.
Fetal kick counts are not a reliable indicator of fetal well-being in the third trimester.
It is not important to do kick counts because you have a low-risk pregnancy.
The Correct Answer is A
Choice A Reason: Fetal movements are an indicator of fetal well-being. You should count twice a day, and you should feel ten fetal movements in 2 hours. This is because this response provides accurate and clear instructions on how to perform kick counts, which are a simple and non-invasive method of monitoring fetal activity and health. Kick counts can help detect changes in fetal movement paterns that may indicate fetal distress or hypoxia.
Choice B Reason: Here is a computer printed information packet on how to do kick counts. This is an insufficient answer that does not address the patient's question or demonstrate effective communication skills. Providing writen information alone may not ensure the patient's understanding or compliance with kick counts.
Choice C Reason: Fetal kick counts are not a reliable indicator of fetal well-being in the third trimester. This is an incorrect answer that contradicts the evidence and guidelines on kick counts. Kick counts are recommended for all pregnant women, especially in the third trimester, when fetal movements are more noticeable and consistent.
Choice D Reason: It is not important to do kick counts because you have a low-risk pregnancy. This is an incorrect answer that discourages the patient from performing kick counts and may give her a false sense of security. Kick counts are important for all pregnant women, regardless of their risk status, as they can help identify potential problems that may require further evaluation or intervention.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A Reason: Vascular spider veins. This is an incorrect answer that refers to a different skin change that occurs during pregnancy, which affects the blood vessels, not the pigment. Vascular spider veins are small red or purple clusters of blood vessels that appear on the skin, especially on the face, neck, chest, or legs. Vascular spider veins are caused by increased blood volume and hormonal changes, which dilate and rupture the capillaries. Vascular spider veins are harmless and usually disappear after delivery.
Choice B Reason: Linea nigra. This is because linea nigra is a term that refers to a darkened vertical line that appears on the abdomen during pregnancy, which runs from the umbilicus to the pubis. Linea nigra is caused by increased production of melanin, which is a pigment that gives color to the skin and hair. Linea nigra is more common and noticeable in women with darker skin tones, and it usually fades after delivery.
Choice C Reason: Melasma. This is an incorrect answer that refers to a different skin change that occurs during pregnancy, which affects the pigment, but not in a linear patern. Melasma is a term that refers to patches of brown or gray-brown discoloration that appear on the face, especially on the forehead, cheeks, nose, or upper lip. Melasma is also caused by increased production of melanin, but it is influenced by sun exposure and genetic factors. Melasma is also known as chloasma or the mask of pregnancy, and it may persist after delivery.
Choice D Reason: Striae gravidarum. This is an incorrect answer that refers to a different skin change that occurs during pregnancy, which affects the connective tissue, not the pigment. Striae gravidarum are stretch marks that appear on the skin, especially on the abdomen, breasts, hips, or thighs. Striae gravidarum are caused by rapid growth and stretching of the skin, which damage the collagen and elastin fibers. Striae gravidarum are initially red or purple, but they fade to white or silver after delivery.
Correct Answer is D
Explanation
Choice A Reason: Moderate amounts of deep red lochia. This is not a finding that would warrant further investigation, but rather a normal finding for the early postpartum period. Lochia is the vaginal discharge that occurs after delivery, which consists of blood, mucus, and tissue from the uterus. Lochia is usually deep red in color and moderate in amount for the first few days after delivery.
Choice B Reason: Sweating while afebrile. This is not a finding that would warrant further investigation, but rather a common occurrence in the postpartum period. Sweating is a mechanism of thermoregulation that helps the body eliminate excess fluid and electrolytes that were retained during pregnancy. Sweating does not necessarily indicate fever or infection.
Choice C Reason: Voiding 350 mL of blood-tinged urine. This is not a finding that would warrant further investigation, but rather an expected outcome for the postpartum period. Voiding large amounts of urine is normal in the postpartum period, as the body eliminates the excess fluid that was accumulated during pregnancy. Blood-tinged urine may be due to trauma or irritation of the urinary tract during labor or delivery, which usually resolves within a few days.
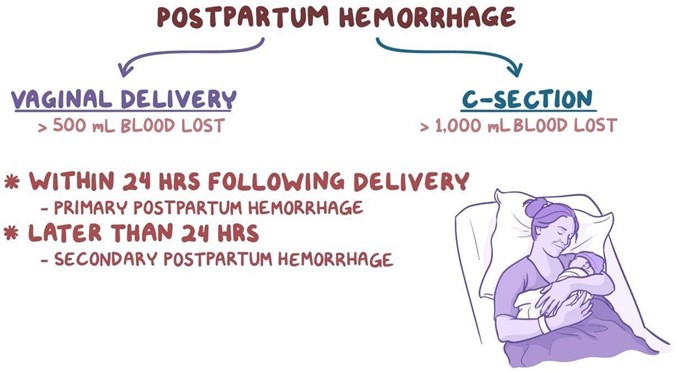
Choice D Reason: Heart rate of 115 beats/minute. This is because a heart rate of 115 beats/minute is higher than the normal range for an adult, which is 60 to 100 beats/minute. A high heart rate may indicate postpartum hemorrhage, infection, pain, anxiety, or dehydration. The nurse should further assess the client for other signs and symptoms of these conditions and notify the physician if necessary.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
