A client with left lower lobe pneumonia has activity intolerance related to impaired oxygen supply and demand as evidenced by fatigue, dyspnea, and difficulty performing self-care. Which expected outcome must be included in the care plan related to this problem? The client will:
Have a pulse oximetry reading of 95% or greater by discharge.
Exhibit a respiratory rate of 12-20/minute by discharge.
Perform self-care activity without dyspnea by discharge.
Have clear breath sounds bilaterally by discharge.
The Correct Answer is C
Choice A reason:
Have a pulse oximetry reading of 95% or greater by discharge: While maintaining a pulse oximetry reading of 95% or greater is important, it may not fully address the client’s activity intolerance. Pulse oximetry measures the oxygen saturation in the blood, and normal readings typically range from 95% to 100%. However, achieving this reading alone does not ensure that the client can perform activities without experiencing dyspnea or fatigue.
Choice B reason:
Exhibit a respiratory rate of 12-20/minute by discharge: A normal respiratory rate for adults is between 12 and 20 breaths per minute. While this is a good indicator of respiratory function, it does not directly address the client’s ability to perform self-care activities without dyspnea. The goal should focus on the client’s functional ability rather than just physiological parameters.
Choice C reason:
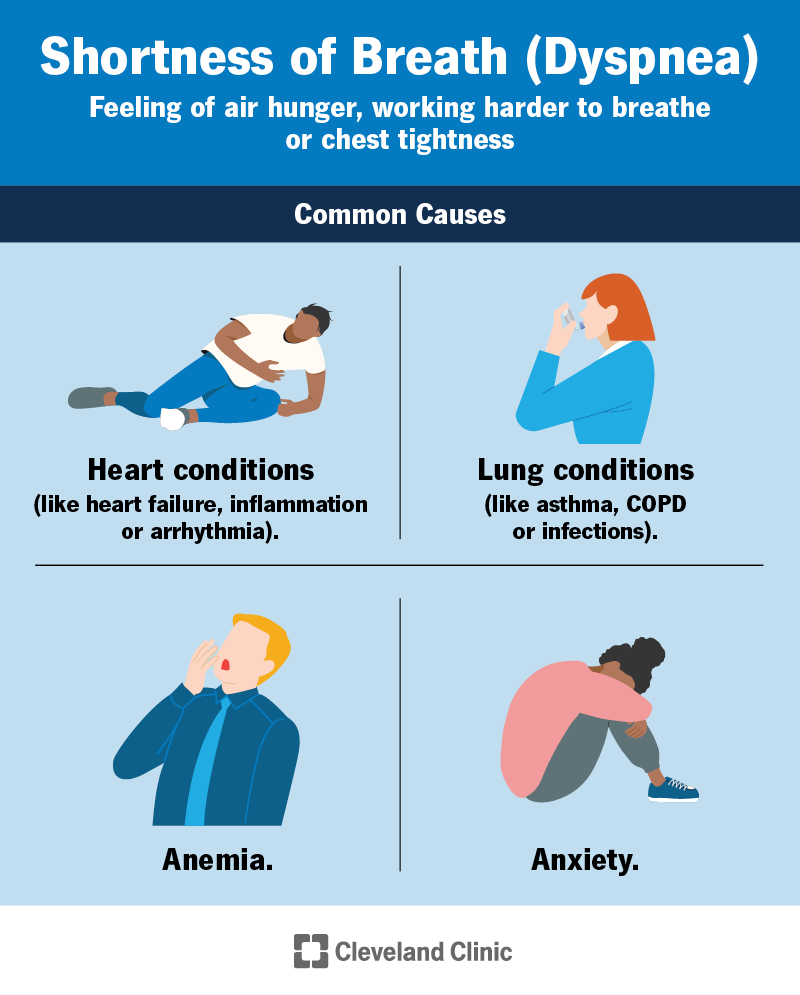
Perform self-care activity without dyspnea by discharge: This outcome directly addresses the client’s activity intolerance. Dyspnea, or difficulty breathing, is a significant symptom that affects the client’s ability to perform daily activities. By setting a goal for the client to perform self-care activities without dyspnea, the care plan focuses on improving the client’s functional status and quality of life.
Choice D reason:
Have clear breath sounds bilaterally by discharge: Clear breath sounds are an important indicator of improved lung function and resolution of pneumonia. However, this outcome does not specifically address the client’s activity intolerance. While clear breath sounds are desirable, the primary goal should be to ensure the client can perform activities without experiencing dyspnea.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A reason:
Fever and bradypnea are not typical manifestations of asthma. Fever is more commonly associated with infections, and bradypnea (abnormally slow breathing) is not a characteristic symptom of asthma.
Choice B reason:
Dyspnea (shortness of breath) and wheezing are hallmark symptoms of asthma. Asthma is characterized by inflammation and narrowing of the airways, which leads to difficulty breathing and a whistling sound (wheezing) when exhaling. These symptoms are often triggered by allergens, exercise, or respiratory infections.
Choice C reason:
Crackles and a productive cough are more indicative of conditions like pneumonia or chronic bronchitis rather than asthma. Asthma typically involves a dry cough rather than a productive one.
Choice D reason:
A normal chest shape and orthopnea (difficulty breathing when lying flat) are not specific to asthma. While some individuals with severe asthma may develop a barrel chest over time due to chronic overinflation of the lungs, this is not a typical early manifestation.
Correct Answer is ["0.5"]
Explanation
Step 1: Convert the prescribed dose from mcg to mg.
- 235 mcg ÷ 1000 = 0.235 mg
Step 2: Determine the strength of the available tablet.
- Available strength = 0.5 mg per tablet
Step 3: Calculate the number of tablets needed.
- Number of tablets = 0.235 mg ÷ 0.5 mg/tablet
Step 4: Perform the division.
- 0.235 ÷ 0.5 = 0.47
Step 5: Round the answer to the nearest tenth.
- 0.47 rounded to the nearest tenth = 0.5
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
