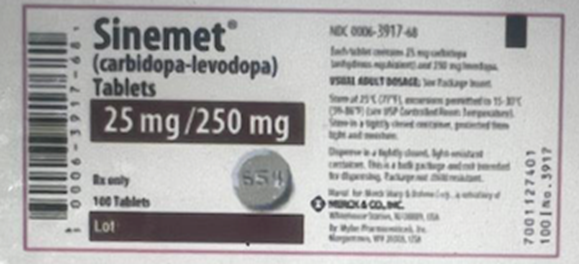
A client with Parkinson's disease is prescribed carbidopa-levadopa [Sinemet]. Which of the following side effects does the nurse recognize can occur with this medication?
Jaundice
Hyperglycemia
Hypertension
Orthostatic hypotension
The Correct Answer is D
A) Jaundice:
Carbidopa-levodopa works by increasing dopamine levels in the brain to help alleviate symptoms of Parkinson's disease, but it is not typically associated with liver dysfunction that would lead to jaundice. If jaundice were to occur, it could indicate liver problems, which would need to be evaluated further, but this is not a typical side effect of Sinemet.
B) Hyperglycemia:
Sinemet primarily affects dopamine levels in the brain and does not have a direct impact on blood sugar regulation. However, long-term use of certain medications, especially corticosteroids or other specific treatments, can affect glucose levels, but carbidopa-levodopa is not typically linked to hyperglycemia.
C) Hypertension:
Carbidopa-levodopa may lead to fluctuations in blood pressure, including lowering blood pressure, especially when the patient is changing positions. However, hypertension is not a typical response to this medication. Instead, patients may experience orthostatic hypotension, which is more common with carbidopa-levodopa.
D) Orthostatic hypotension:
Orthostatic hypotension is a well-recognized and common side effect of carbidopa-levodopa. This occurs because Sinemet affects the autonomic nervous system, which can cause a decrease in blood pressure when moving from a sitting or lying position to standing. Patients on carbidopa-levodopa should be advised to rise slowly to minimize the risk of dizziness or fainting due to orthostatic hypotension.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
A) Normal saline 1 liter to client who is dehydrated:
Administering normal saline to a dehydrated client is an important task, as it helps to restore fluid balance and improve circulatory volume. However, while rehydration is critical, it is not an immediate, life-threatening priority compared to other interventions. The nurse should begin this infusion after addressing more urgent needs such as severe chest pain, which could indicate a cardiac emergency.
B) Morphine sulfate 4mg intravenously (IV) now for the client experiencing incisional pain:
Morphine is a potent analgesic, and relieving pain for postoperative patients is essential for comfort and recovery. However, incisional pain, although important to address, is not life-threatening in this scenario. The client with chest pain should be prioritized because chest pain could indicate a myocardial infarction (MI) or other serious cardiac event that requires immediate intervention.
C) Nitroglycerin (Nitrostat) 0.4 mg sublingually (SL) stat for the client experiencing crushing chest pain:
Crushing chest pain is a classic symptom of acute myocardial infarction (MI), a life-threatening condition that requires immediate intervention. Nitroglycerin is used to relieve chest pain associated with angina or MI by dilating the coronary arteries and improving blood flow to the heart. In this case, chest pain is the most critical symptom, and immediate treatment is necessary to reduce the risk of further cardiac damage or complications.
D) Lorazepam 2 mg IV now for the client who is anxious and restless:
While lorazepam is an effective medication for anxiety and restlessness, it is not the most urgent medication in this case. The client’s anxiety should be addressed, but it does not pose an immediate threat to life. Anxiety can generally be managed after more acute, life-threatening conditions (such as chest pain) are stabilized.
Correct Answer is A
Explanation
A) Respiratory rate of 8 bpm:
This a sign of respiratory depression, which can occur in patients with chronic obstructive pulmonary disease (COPD) who are receiving high-flow oxygen. In COPD patients, particularly those with chronic hypercapnia (elevated carbon dioxide), the body may become less sensitive to CO2 buildup and more reliant on low oxygen levels to trigger the respiratory drive. If oxygen is administered at high flow rate, it can reduce the stimulus for breathing, leading to hypoventilation or even respiratory arrest.
B) A large barrel chest:
A barrel chest is a common physical finding in patients with chronic COPD due to the hyperinflation of the lungs. This is a result of air trapping, which is a hallmark of COPD. While it indicates the long-term effects of COPD, it does not require immediate intervention. It is a chronic sign and not an acute or urgent concern unless accompanied by other signs of acute respiratory distress.
C) Fine crackles:
Fine crackles (or rales) on auscultation can be indicative of fluid in the lungs and may suggest conditions such as pulmonary edema, heart failure, or pneumonia. While crackles could be concerning, they are not as immediately life-threatening as a respiratory rate of 8 bpm. In a patient with COPD, crackles might indicate worsening of their condition, possibly due to an infection or fluid overload, but the priority would still be to assess the patient's breathing and ventilation status first.
D) The patient assumes the orthopneic position:
The orthopneic position (sitting upright or leaning forward) is a common way for patients with COPD to relieve shortness of breath. It is a compensatory action to help improve lung expansion and facilitate breathing. While it is a sign of respiratory distress, it is not an immediate emergency. Many COPD patients use this position to cope with chronic difficulty breathing.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
