A nurse is assessing a full-term newborn upon admission to the nursery. Which of the following clinical findings should the nurse report to the provider?
Rust-stained urine.
Single palmar creases.
Subconjunctival hemorrhage.
Transient circumoral cyanosis
The Correct Answer is B
The correct answer is choice B. Single palmar creases.
Choice A rationale:
Rust-stained urine is typically due to urate crystals and is common in newborns. It usually resolves on its own and is not a cause for concern.
Choice B rationale:
Single palmar creases can be associated with certain genetic conditions, such as Down syndrome. This finding should be reported to the provider for further evaluation.
Choice C rationale:
Subconjunctival hemorrhage is a common finding in newborns due to the pressure changes during delivery. It usually resolves without intervention and is not typically a cause for concern.
Choice D rationale:
Transient circumoral cyanosis is often seen in newborns and can occur when the baby is crying or feeding. It usually resolves on its own and is not typically a cause for concern.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Maternal hypotension is a common complication of spinal anesthesia for cesarean section, and it can cause adverse effects on the mother and the fetus, such as nausea, vomiting, dizziness, decreased placental perfusion, fetal acidosis, and fetal distress¹². To prevent or treat maternal hypotension, various techniques have been used, such as fluid preloading or co-loading, vasopressors, lower limb compression devices, and left lateral tilt position¹². Among these, fluid administration is the most widely used and recommended
intervention¹²³. A bolus infusion of lactated Ringer's or other crystalloid solution can increase the intravascular volume and cardiac output, and counteract the decrease in blood pressure caused by spinal anaesthesia¹²³. The optimal timing and amount of fluid administration may vary depending on the individual patient's condition and response, but generally a bolus of 10 to 20 mL/kg is suggested before or during spinal anaesthesia¹²³.
The other options are incorrect because:
b) Applying oxygen via nonrebreather face mask at 2 L/min is not an effective intervention for maternal hypotension. Oxygen supplementation may be beneficial for improving fetal oxygenation in case of fetal distress, but it does not directly increase maternal blood pressure or cardiac output¹². Moreover, 2 L/min is a low flow rate for a nonrebreather face mask, which requires at least 10 L/min to deliver high concentrations of oxygen⁴.
c) Positioning the client in a knee-chest position is not a recommended intervention for maternal hypotension. This position may increase venous return and cardiac output in some cases, but it also increases intra-abdominal pressure and reduces uterine blood flow, which can compromise fetal oxygenation and well-being. A left lateral tilt position of 15 to 30 degrees is preferred to avoid aortocaval compression and improve placental perfusion¹².
d) Giving terbutaline subcutaneously is not an appropriate intervention for maternal hypotension. Terbutaline is a beta-agonist that relaxes the uterine smooth muscle and prevents preterm labor contractions. It has no direct effect on maternal blood pressure or cardiac output, and it may cause maternal tachycardia, palpitations, tremors, and hypokalemia as side effects. Vasopressors such as ephedrine or phenylephrine are more effective and safer drugs for treating maternal hypotension¹².

Correct Answer is C
Explanation
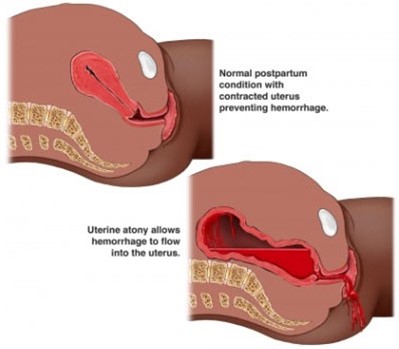
Postpartum hemorrhage (PPH) is severe vaginal bleeding after childbirth. It can occur within 24 hours of delivery (primary PPH) or up to 12 weeks postpartum (secondary PPH) ¹. PPH can cause serious complications and even death if not treated promptly and effectively¹.
The client in the question is at risk for PPH because she has a rapid labor and a high degree of cervical dilation. These factors can cause uterine atony, which is the failure of the uterus to contract and compress the blood vessels after delivery. Uterine atony is the most common cause of PPH, accounting for up to 80% of cases². Other risk factors for PPH include placental abruption, placenta previa, overdistended uterus, multiple pregnancy, prolonged labor, operative delivery, retained placenta, coagulation disorders, and infection²³.
a) Hyperemesis gravidarum is a condition of severe nausea and vomiting during pregnancy that can cause dehydration, electrolyte imbalance, weight loss, and nutritional deficiencies. It usually occurs in the first trimester and resolves by the second trimester. It is not related to PPH⁴.
b) Ectopic pregnancy is a condition where the fertilized egg implants outside the uterus, usually in the fallopian tube. It can cause abdominal pain, vaginal bleeding, and rupture of the tube. It is a medical emergency that requires prompt diagnosis and treatment. It occurs in early pregnancy and cannot be diagnosed at 12 weeks of gestation by amniocentesis.
d) Incompetent cervix is a condition where the cervix dilates prematurely and painlessly during pregnancy, leading to preterm labor and delivery or pregnancy loss. It usually occurs in the second trimester and can be treated with cervical cerclage or progesterone. It is not associated with PPH.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
