A nurse is assisting with the care of a postoperative client who is receiving a unit of packed RBCs. Which data should the nurse recognize as an indication of a septic reaction to the blood transfusion?
Hypertension
Distended neck veins
Polyuria
Vomiting
The Correct Answer is D
Choice A reason: Hypertension is not a sign of a septic reaction, but rather a sign of a hypertensive or circulatory overload reaction to the blood transfusion.
Choice B reason: Distended neck veins are not a sign of a septic reaction, but rather a sign of a circulatory overload or cardiac failure reaction to the blood transfusion.
Choice C reason: Polyuria is not a sign of a septic reaction, but rather a sign of a hemolytic or renal failure reaction to the blood transfusion.
Choice D reason: Vomiting is a sign of a septic reaction, which occurs when the blood transfusion is contaminated with bacteria. Other signs of a septic reaction include fever, chills, hypotension, and shock.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A: This is incorrect. Vegetable shortening is high in saturated fat and trans fat, which can increase the risk of cardiovascular disease by raising the LDL (bad) cholesterol and lowering the HDL (good) cholesterol.
Choice B: This is incorrect. Lard is animal fat that is high in saturated fat and cholesterol, which can also increase the risk of cardiovascular disease by raising the LDL cholesterol and lowering the HDL cholesterol.
Choice C: This is correct. Canola oil is low in saturated fat and high in monounsaturated fat and omega-3 fatty acids, which can lower the risk of cardiovascular disease by lowering the LDL cholesterol and raising the HDL cholesterol.
Choice D: This is incorrect. Butter is dairy fat that is high in saturated fat and cholesterol, which can also increase the risk of cardiovascular disease by raising the LDL cholesterol and lowering the HDL cholesterol
Correct Answer is D
Explanation
Choice A reason: PaO2 85 mmHg is within the normal range of 80 to 100 mmHg and does not indicate any hypoxemia or oxygen deficiency.
Choice B reason: pH 7.47 is within the normal range of 7.35 to 7.45 and does not indicate any acid-base imbalance.
Choice C reason: HCO3 25 mEq/L is within the normal range of 22 to 26 mEq/L and does not indicate any metabolic disturbance.
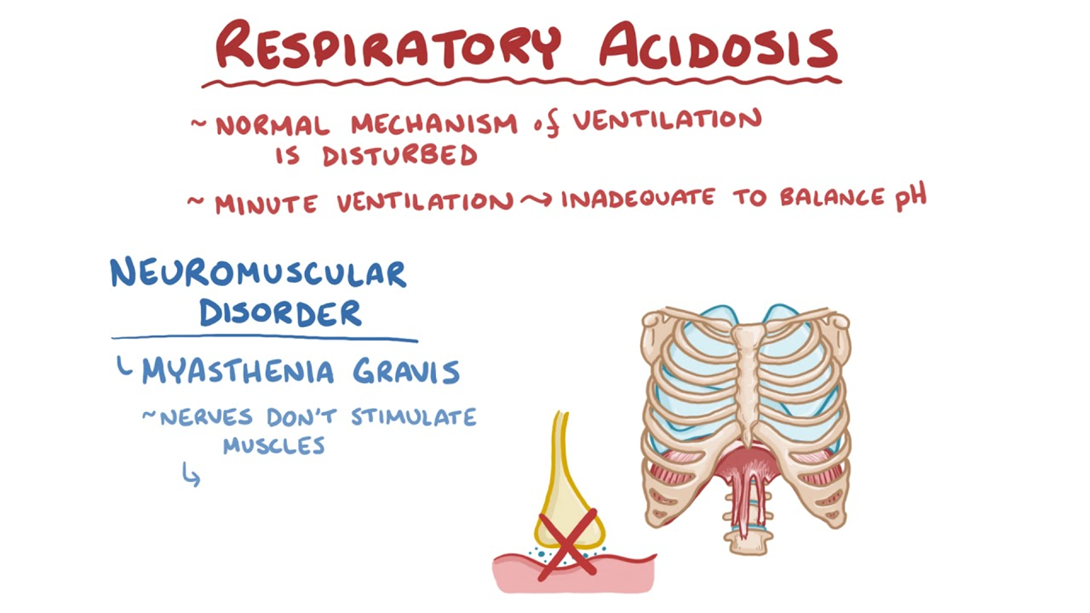
Choice D reason: PaCO2 55 mmHg is above the normal range of 35 to 45 mmHg and indicates respiratory acidosis, which is a condition where the lungs cannot eliminate enough carbon dioxide and the blood becomes too acidic. This can be caused by pneumonia, which can impair gas exchange and ventilation.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
