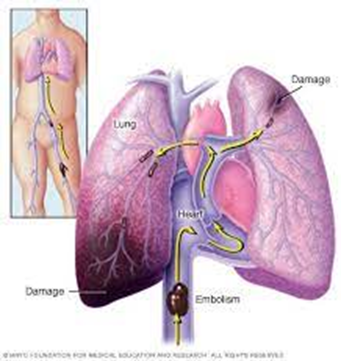
A nurse is caring for a client who has a pulmonary embolism. The nurse should identify that the release of inflammatory mediators leads to which of the following pathologic findings?
Decreased pulmonary vascular resistance
Hypercapnia
Hypoventilation
Respiratory alkalosis
The Correct Answer is D
Correct answer: D
Choice A Reason:
Decreased pulmonary vascular resistance is incorrect. Inflammatory mediators released in response to a pulmonary embolism can lead to vasoconstriction and increased pulmonary vascular resistance. This is part of the body's response to redirect blood flow away from the affected area of the lung and maintain adequate perfusion to other areas.
Choice B Reason:
Hypercapnia is incorrect. Hypercapnia refers to elevated levels of carbon dioxide (CO2) in the blood. Hypocapnia usually is present with embolism; hypercapnia, on the other hand, is rare.
Choice C Reason:
Hypoventilation is incorrect. Hypoventilation occurs when there is inadequate ventilation of the lungs relative to metabolic demands. In the context of a pulmonary embolism, hypoventilation can occur due to factors such as pain, respiratory muscle fatigue, or impaired gas exchange, all of which can be influenced by the release of inflammatory mediators.
Choice D Reason:
Respiratory alkalosis is correct. In response to the blockage and the resulting inflammation, the body often increases the respiratory rate as a compensatory mechanism to maintain adequate oxygen levels and remove carbon dioxide. Due to the increased breathing rate, there is excessive exhalation of carbon dioxide, leading to a decrease in the partial pressure of CO2 in the blood. This results in an increase in blood pH, causing respiratory alkalosis.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A Reason:
The client should maintain systolic BP between 120 and 129 mm Hg. This option aligns with current guidelines for blood pressure management following a transient ischemic attack (TIA). Tight blood pressure control is recommended to reduce the risk of recurrent cerebrovascular events, such as stroke. Maintaining systolic blood pressure (SBP) between 120 and 129 mm Hg has been associated with significant risk reduction in stroke recurrence compared to higher blood pressure targets. Therefore, this option reflects the recommended approach for blood pressure management in individuals with a history of TIA.
Choice B Reason:
The client should maintain systolic BP between 136 and 140 mm Hg: This option suggests a systolic blood pressure (SBP) range that is higher than the recommended target for blood pressure management following a TIA. Allowing SBP to remain in the range of 136 to 140 mm Hg may pose an increased risk of recurrent cerebrovascular events compared to tighter blood pressure control.
Choice C Reason:
The client should maintain systolic BP between 141 and 145 mm Hg. Similarly, this option proposes a systolic blood pressure (SBP) range that is higher than the recommended target for blood pressure management following a TIA. Allowing SBP to remain in the range of 141 to 145 mm Hg may not provide adequate protection against stroke recurrence compared to tighter blood pressure control.
Choice D Reason:
The client should maintain systolic BP between 130 and 135 mm Hg. While this option suggests a systolic blood pressure (SBP) range that is closer to the recommended target compared to options B and C, it still falls slightly above the optimal range for blood pressure management following a TIA. Tighter blood pressure control, ideally below 130 mm Hg, is typically preferred to reduce the risk of recurrent cerebrovascular events.
Correct Answer is ["A","B","D","E"]
Explanation
Choice A Reason:
Memory loss is correct. Memory loss can occur in individuals with PML due to damage to the white matter of the brain caused by the JC virus infection. This damage can affect cognitive function, including memory.
Choice B Reason:
Clumsiness is correct. Clumsiness or lack of coordination is a common neurological symptom of PML. It can result from damage to areas of the brain responsible for motor function and coordination.
Choice C Reason:
Tardive dyskinesia is incorrect. Tardive dyskinesia is a movement disorder characterized by involuntary, repetitive movements, often involving the face, lips, tongue, and limbs. While tardive dyskinesia can occur as a side effect of certain medications, it is not typically associated with PML.
Choice D Reason:
Seizures is correct. Seizures can occur in individuals with PML due to the involvement of the brain's white matter by the JC virus infection. Seizures may present as sudden, uncontrolled movements, altered consciousness, or other neurological symptoms.
Choice E Reason:
Vision difficulty is correct. Vision difficulties, including blurred vision, visual field deficits, and other visual disturbances, are common manifestations of PML. Damage to the optic nerves or areas of the brain involved in visual processing can result in vision difficulties.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
