A nurse is caring for a client who is 1 day postoperative following an open thoracotomy. The client is receiving oxygen mist at 40% by face tent. The client's SPO2 is 89-96%. ABG results are: pH 7.31, PaO2 93 mm Hg, PCO2 5O mm Hg, HCO3 25 mEq/L. Which of the following is an appropriate action by the nurse?
Position the client prone and have the respiratory therapist perform postural drainage.
Place the client in high-Fowler's position and encourage the use of incentive spirometer and coughing.
Increase oxygen to 70%.
Switch oxygen to a nonrebreather mask.
The Correct Answer is B
A. Prone positioning and postural drainage are typically not appropriate interventions for a client 1 day postoperative following an open thoracotomy, as this could place stress on the incision site and cause discomfort or injury.
B. High-Fowler's position facilitates lung expansion, which can improve ventilation and oxygenation. Encouraging the use of an incentive spirometer and promoting coughing helps clear secretions and expand the lungs, addressing the mild respiratory acidosis indicated by the ABG results (pH 7.31 and PaCO2 50 mm Hg).
C. Increasing oxygen to 70% is not appropriate, as the PaO2 level is within normal limits (93 mm Hg). The client's issue appears to be related more to ventilation (indicated by the elevated PaCO2) rather than oxygenation, so additional oxygen would not address the underlying cause and could lead to oxygen toxicity if used long-term.
D. A nonrebreather mask delivers a high concentration of oxygen, which is not necessary in this case since the client’s PaO2 is already adequate. The primary issue is not a lack of oxygen but rather the retention of CO2, so promoting ventilation and lung expansion through positioning and respiratory exercises is more appropriate.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
A. Evidence-based practice:
Evidence-based practice (EBP) involves integrating the best available evidence from research, clinical expertise, and patient preferences and values to inform nursing practice. In perioperative nursing, EBP is important for making informed decisions about preoperative, intraoperative, and postoperative care protocols. For example, using evidence-based guidelines for surgical site infection prevention, pain management strategies, and postoperative care protocols can improve patient outcomes and safety.
B. Informatics:
Informatics refers to the use of information technology and data management systems to support nursing practice, education, research, and patient care. In perioperative nursing, informatics plays a crucial role in managing electronic health records (EHRs), accessing patient data, documenting care, and communicating with interdisciplinary team members. It also includes utilizing perioperative information systems for surgical scheduling, anesthesia records, and tracking patient progress during surgery.
C. Quality improvement:
Quality improvement (QI) involves systematic processes to monitor, assess, and improve the quality of healthcare services. In perioperative nursing, QI initiatives focus on enhancing patient safety, optimizing surgical outcomes, reducing complications, and improving efficiency in perioperative processes. Nurses participate in QI projects by analyzing data, identifying areas for improvement, implementing evidence-based practices, and evaluating the impact of interventions on patient care and outcomes.
D. Safety:
Safety is a fundamental QSEN competency, particularly critical in perioperative nursing care. Perioperative nurses are responsible for ensuring the safety of patients during all phases of surgery, including preoperative assessment, intraoperative care, and postoperative recovery. This includes measures such as verifying patient identity and surgical site, preventing surgical errors (e.g., wrong-site surgery), maintaining aseptic techniques to prevent infections, preventing falls and injuries, managing anesthesia safely, and adhering to protocols for safe medication administration and equipment use.
Correct Answer is D
Explanation
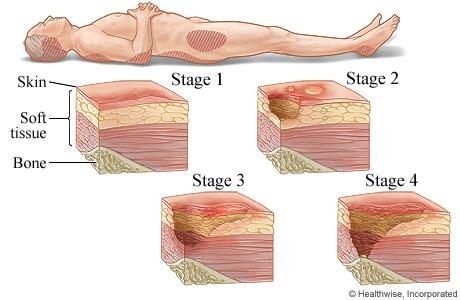
A. Stage III pressure injury
Stage III pressure injuries involve full-thickness skin loss, extending into the subcutaneous tissue but not through the fascia. These wounds typically present as deep craters and may involve undermining or tunneling. Non-blanchable erythema alone without visible skin loss is not characteristic of a Stage III pressure injury.
B. Stage IV pressure injury
Stage IV pressure injuries are the most severe and involve full-thickness tissue loss with exposed bone, tendon, or muscle. These wounds often have extensive tissue damage and can be difficult to manage. Again, non-blanchable erythema without visible skin loss is not indicative of a Stage IV pressure injury.
C. Stage II pressure injury
Stage II pressure injuries involve partial-thickness skin loss with damage to the epidermis and possibly the dermis. These wounds often present as shallow open ulcers or blisters and may have characteristics such as intact or ruptured blisters. While Stage II injuries can present with erythema, non-blanchable erythema specifically indicates a Stage I injury.
D. Stage I pressure injury
Stage I pressure injuries are the earliest stage and involve non-blanchable erythema of intact skin. The skin may be warmer or cooler than surrounding tissue and may have changes in sensation. There is no visible skin loss at this stage, but the area is at risk for further injury if pressure is not relieved. Therefore, non-blanchable erythema on the heels most likely indicates a Stage I pressure injury.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
