A nurse is caring for a client that is immobile. The nurse recognizes that the appearance of non-blanchable erythema on the heels most likely indicates which of the following stages of pressure injuries?
Stage III pressure injury
Stage IV pressure injury
Stage II pressure injury
Stage I pressure injury
The Correct Answer is D
A. Stage III pressure injury
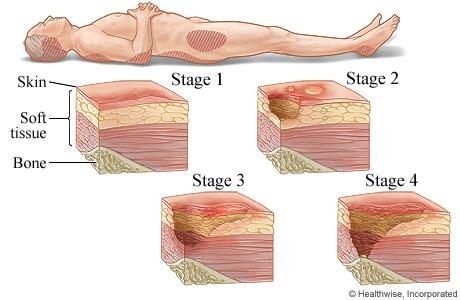
Stage III pressure injuries involve full-thickness skin loss, extending into the subcutaneous tissue but not through the fascia. These wounds typically present as deep craters and may involve undermining or tunneling. Non-blanchable erythema alone without visible skin loss is not characteristic of a Stage III pressure injury.
B. Stage IV pressure injury
Stage IV pressure injuries are the most severe and involve full-thickness tissue loss with exposed bone, tendon, or muscle. These wounds often have extensive tissue damage and can be difficult to manage. Again, non-blanchable erythema without visible skin loss is not indicative of a Stage IV pressure injury.
C. Stage II pressure injury
Stage II pressure injuries involve partial-thickness skin loss with damage to the epidermis and possibly the dermis. These wounds often present as shallow open ulcers or blisters and may have characteristics such as intact or ruptured blisters. While Stage II injuries can present with erythema, non-blanchable erythema specifically indicates a Stage I injury.
D. Stage I pressure injury
Stage I pressure injuries are the earliest stage and involve non-blanchable erythema of intact skin. The skin may be warmer or cooler than surrounding tissue and may have changes in sensation. There is no visible skin loss at this stage, but the area is at risk for further injury if pressure is not relieved. Therefore, non-blanchable erythema on the heels most likely indicates a Stage I pressure injury.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
A. Provide a heart-healthy low-potassium diet:
While a heart-healthy low-potassium diet is essential for managing chronic hyperkalemia and preventing future occurrences, it is not the first intervention to implement in a patient with a serum potassium level of 7.5 mEq/L and exhibiting cardiovascular changes. The effects of dietary changes on serum potassium levels are gradual and may take days to have a significant impact. In an acute situation like this, immediate interventions are needed to rapidly lower potassium levels and address the associated cardiovascular risks.
B. Prepare to administer sodium polystyrene sulfate 15g by mouth:
Sodium polystyrene sulfate is a medication used to exchange sodium for potassium in the gastrointestinal tract, effectively lowering serum potassium levels over hours to days. While it is a valid treatment for hyperkalemia, its onset of action is not immediate enough to address the urgent cardiovascular changes seen in severe hyperkalemia. Therefore, it is not the first-line intervention in this scenario.
C. Prepare the patient for hemodialysis treatment:
Hemodialysis is an effective method for rapidly lowering serum potassium levels in cases of severe hyperkalemia. However, it is a more invasive and time-consuming procedure that requires preparation, including vascular access and dialysis setup. It is typically reserved for situations where other interventions have failed or in patients with severe or refractory hyperkalemia. In the context of this scenario, where the patient has a serum potassium level of 7.5 mEq/L and is exhibiting cardiovascular changes, hemodialysis may be considered if initial interventions are not successful, but it is not the first action to implement.
Correct Answer is C
Explanation
A. Inform the client that the recovery nurse will instruct them how to manage postoperative pain:
This is an important aspect of postoperative care, but it is typically addressed by the post-anesthesia care unit (PACU) or recovery nurse after surgery rather than in the preoperative education phase. While pain management education is crucial, the focus of preoperative education is usually on what to expect before, during, and immediately after surgery.
B. Remind the client they will return to their room after surgery:
This information is part of the preoperative instructions and helps alleviate anxiety by providing clarity about the post-surgical process. However, it may not be the most critical aspect of preoperative education compared to other options.
C. Provide instructions about how to cough and deep breathe effectively:
This is a key nursing intervention to include in preoperative education. Teaching the client how to cough and deep breathe effectively helps prevent postoperative complications such as atelectasis and pneumonia. These breathing techniques are typically taught preoperatively to ensure the client understands and can perform them correctly after surgery.
D. Notify the client that they will receive a food tray in the recovery room:
While it's important for the client to understand the postoperative diet plan, including any dietary restrictions or instructions, this information is usually provided after surgery rather than in the preoperative education phase.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
