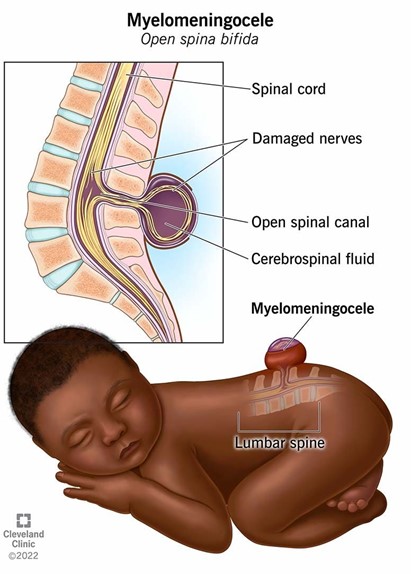
A nurse is planning care immediately following birth for a newborn who has a myelomeningocele that is leaking cerebrospinal fluid. Which of the following actions should the nurse include in the plan of care?
Cleanse the site with povidone-iodine.
Administer broad-spectrum antibiotics.
Prepare for surgical closure after 72 hours.
Monitor the rectal temperature every 4 hours.
The Correct Answer is B
A. Using povidone-iodine on the site of a myelomeningocele is not recommended as it can be irritating to the tissue and might not be safe for use on open neural tissue. The focus should be on preventing infection through other means.
B. Administering broad-spectrum antibiotics is crucial as the cerebrospinal fluid (CSF) leak increases the risk of infection, such as meningitis. Antibiotics help protect the newborn from potentially serious infections until surgical repair can be performed.
C. Surgical closure of a myelomeningocele is typically done as soon as possible, often within 24-48 hours after birth, to minimize the risk of infection and further damage to the exposed spinal cord.
D. While monitoring temperature is important, rectal temperature measurement is not recommended for a newborn with a myelomeningocele due to the risk of causing further complications. Axillary temperature measurement would be safer and less invasive.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Preparing a toddler for a new sibling can be challenging, but there are some strategies that can help ease the transition and reduce the risk of jealousy or resentment. One of these strategies is to make any major changes in the toddler's routine or environment well before the baby arrives, such as moving to a new bed, starting preschool, or toilet training. This can help the toddler adjust to the change without feeling displaced or threatened by the baby. It can also prevent the toddler from associating the change with the baby and blaming the baby for it¹².
Moving a toddler to a new bed 2 months before the baby comes home is a good example of this strategy. It gives the toddler enough time to get used to sleeping in a different place and feeling comfortable and secure in it. It also avoids making the toddler feel like they are being kicked out of their bed to make room for the baby. The toddler may even feel proud of having a big-kid bed and being more independent¹².
The other options are not appropriate responses by the nurse because they may have negative effects on the toddler's adjustment to the new sibling:
a) "Let your toddler see you carrying the baby into the home for the first time." This is not a good idea because it may make the toddler feel left out or replaced by the baby. The toddler may not understand why they were not with you when you brought the baby home and may feel hurt or angry. A better option is to have someone else carry the baby into the home while you greet your toddler with a hug and a smile. Then, you can introduce your toddler to their new sibling and involve them in welcoming and caring for the baby¹³.
b) "Avoid bringing your toddler to prenatal visits." This is not a good idea because it may make the toddler feel excluded or curious about what is going on. Bringing your toddler to some of your prenatal visits can help them learn more about the baby and feel more connected to them. You can show your toddler pictures of the baby's development, let them hear the baby's heartbeat, or ask them to help you choose clothes or toys for the baby. However, you should also be prepared for your toddler's possible boredom or impatience during long or boring appointments and bring some snacks or activities to keep them entertained¹⁴.
c) "Require scheduled interactions between the toddler and the baby." This is not a good idea because it may make the toddler feel pressured or resentful toward the baby. Forcing your toddler to interact with the baby when they are not ready or interested can backfire and cause more conflict or distance between them. A better option is to follow your toddler's cues and let them decide how much and when they want to interact with the baby. You can also praise your toddler for any positive interactions they have with the baby, such as giving them a gentle kiss, sharing a toy, or singing a song¹³.
Correct Answer is C
Explanation
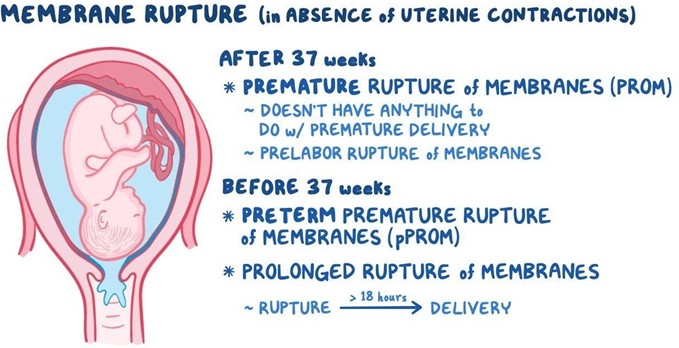
Umbilical cord prolapse is a medical emergency that occurs when the umbilical cord comes out of the uterus with or before the presenting part of the baby. The concern with cord prolapse is that pressure on the cord from the baby will compromise blood flow to the baby. It usually occurs during labor but can occur any time after the rupture of membranes³.
Umbilical cord prolapse can cause fetal hypoxia (lack of oxygen), bradycardia (slow heart rate), acidosis (high acidity in the blood), and death if not treated promptly. The immediate goal of management is to relieve the pressure on the cord and restore blood flow to the baby. The definitive treatment is an emergency cesarean section to deliver the baby as soon as possible¹².
While waiting for the cesarean section, the nurse should take several steps to reduce the risk of fetal
compromise, such as:
- Call for help and notify the provider
- Place the client in a knee-chest, Trendelenburg, or modified Sims position to shift the fetal weight off the
cord
- Exert continuous upward pressure on the presenting part with a sterile gloved hand to lift it away from
the cord
- Administer oxygen to the client at 8 to 10 L/min via a nonrebreather mask
- Administer IV fluids to maintain hydration and blood pressure
- Administer tocolytics (medications that stop uterine contractions) as ordered to reduce cord compression
- Monitor fetal heart rate and uterine activity continuously
- Provide emotional support and reassurance to the client and family
Exerting continuous upward pressure on the presenting part is a critical action that the nurse should take to prevent further cord compression and improve fetal oxygenation. The nurse should insert a sterile gloved hand into the vagina and gently push up on the fetal head or buttocks until delivery. The nurse should not attempt to push the cord back into the uterus or manipulate it in any way, as this could cause more damage or infection¹².
The other options are not actions that the nurse should take:
- a) Place the client in a left-lateral position for 1 hr. after administration. This is not correct because this position does not relieve the pressure on the cord. The client should be placed in a knee-chest, Trendelenburg, or modified Sims position instead.
- b) Initiate oxytocin via continuous IV infusion. This is not correct because oxytocin stimulates uterine contractions, which can worsen cord compression and fetal distress. The nurse should administer tocolytics instead to stop contractions.
- d) Request that the provider insert an intrauterine pressure catheter. This is not correct because an intrauterine pressure catheter is used to measure uterine contractions, not cord prolapse. Inserting a catheter could also increase the risk of infection or injury.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
