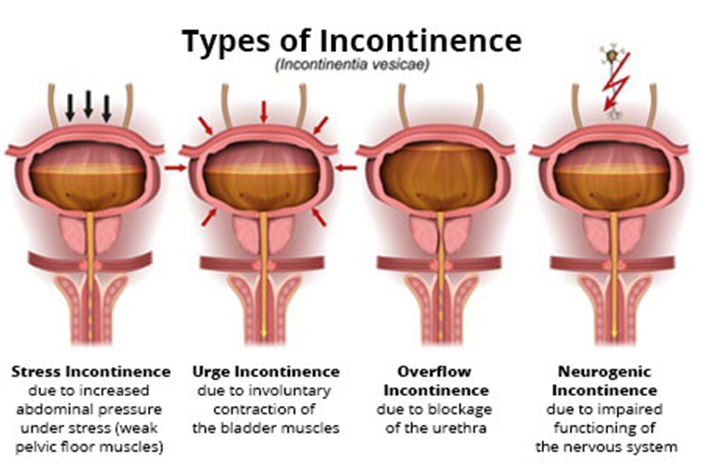
After teaching a local woman's group about incontinence, the nurse determines that the teaching was successful when the group identifies which characteristic of stress incontinence?
developing most often in women in their 30s
feeling a strong need to void
passing a large amount of urine
sneezing as an initiating stimulus
The Correct Answer is D
A. Developing most often in women in their 30s:
Stress incontinence can affect women of various ages, not specifically those in their 30s. While childbirth and hormonal changes associated with aging can increase the risk of stress incontinence, it is not limited to any particular age group.
B. Feeling a strong need to void:
This characteristic is more indicative of urgency incontinence, also known as overactive bladder (OAB), where there is a sudden, strong urge to urinate that is difficult to control. It is different from stress incontinence, which is triggered by physical movements or activities that increase pressure on the bladder.
C. Passing a large amount of urine:
This choice does not specifically describe a characteristic of stress incontinence. Stress incontinence involves the leakage of small amounts of urine during activities such as coughing, sneezing, laughing, or exercising, rather than the passage of a large amount of urine at once.
D. Sneezing as an initiating stimulus:
This is the correct characteristic of stress incontinence. Stress incontinence is characterized by the leakage of urine during physical activities or movements that increase intra-abdominal pressure, such as coughing, sneezing, laughing, lifting, or exercising. Sneezing is a common initiating stimulus for stress incontinence episodes.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
A. Encouraging range-of-motion exercises: Range-of-motion exercises are generally encouraged post-hysterectomy to prevent complications such as blood clots and promote circulation. This action is appropriate and not contraindicated.
B. Ambulating the client: Ambulation is an essential aspect of postoperative care to prevent complications like atelectasis, pneumonia, and deep vein thrombosis (DVT). This action helps improve circulation and aids in the recovery process. It is appropriate and not contraindicated.
C. Applying elasticized stockings: Elasticized stockings, also known as compression stockings, are commonly used postoperatively to prevent deep vein thrombosis (DVT) by promoting blood flow in the legs. However, in the case of abdominal hysterectomy, if the incision site is below the level of the stockings, they may impede circulation to the surgical site and hinder wound healing. Therefore, this action may be contraindicated depending on the specific circumstances of the surgery and incision site.
D. Massaging the client's legs: Massaging the client's legs is generally not recommended post-hysterectomy, especially in the immediate postoperative period. Manipulating the legs could potentially disrupt healing tissues, increase the risk of bleeding, or cause discomfort to the client. Therefore, this action may be contraindicated.
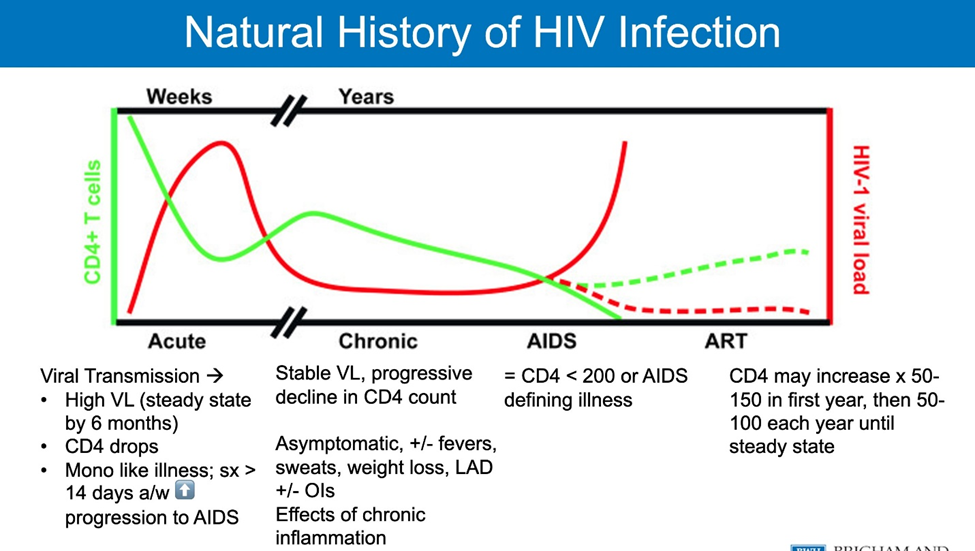
Correct Answer is D
Explanation
A. 1,000 cells/mm3:
A CD4 cell count of 1,000 cells/mm3 is within the normal range for a healthy individual. In HIV-positive individuals, a CD4 count at this level would generally indicate that the immune system is functioning well and has not been significantly compromised by the virus. Therefore, a CD4 count of 1,000 cells/mm3 would not suggest a diagnosis of AIDS.
B. 700 cells/mm3:
Similarly, a CD4 cell count of 700 cells/mm3 is also within the normal range for immune function. While this count may be lower than the typical CD4 count in a healthy individual, it is still considered relatively high and would not indicate immune compromise to the extent seen in AIDS.
C. 450 cells/mm3:
A CD4 cell count of 450 cells/mm3 is also within a range that suggests the immune system is functioning reasonably well. While it may be lower than normal, it is not at a level indicative of severe immune suppression characteristic of AIDS.
D. 200 cells/mm3:
When the CD4 cell count drops below 200 cells/mm3, it indicates significant immune suppression and an increased risk of opportunistic infections. This threshold is used to diagnose AIDS in HIV-positive individuals. At this level, the immune system is severely compromised, leaving the individual vulnerable to various infections and diseases associated with AIDS.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
