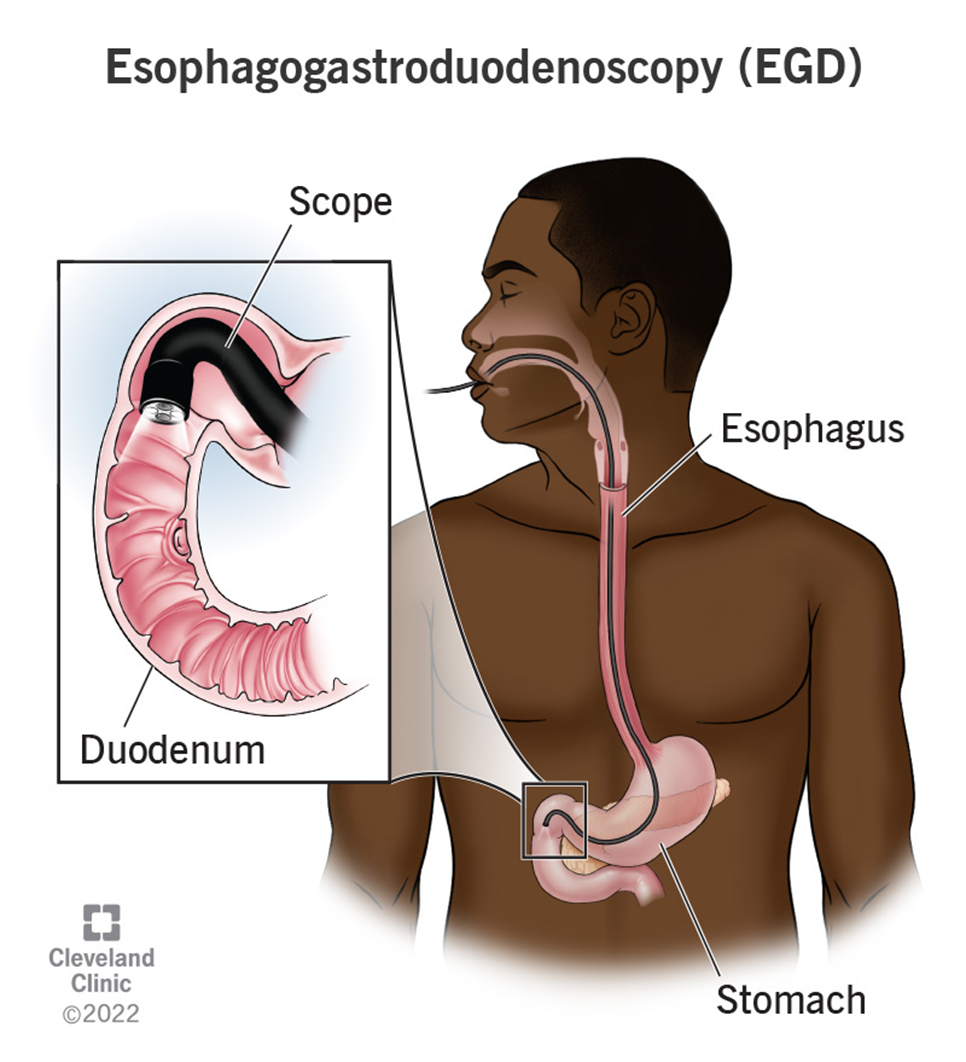
The nurse is caring for a client recovering from an esophagogastroduodenoscopy (EGD). Which of the following client symptoms would require further nursing assessment?
Thirst
Sore throat
Abdominal distention
Drowsiness
The Correct Answer is C
Choice A Reason:
Thirst is a common and expected symptom after an EGD, especially if the client has been fasting before the procedure. It does not typically indicate a complication and can be managed by gradually reintroducing fluids as tolerated. Therefore, thirst does not require further nursing assessment beyond routine post-procedure care.
Choice B Reason:
A sore throat is also a common symptom following an EGD. The procedure involves passing an endoscope through the throat, which can cause temporary irritation and discomfort. This symptom usually resolves on its own within a few days and does not indicate a serious complication. Therefore, a sore throat does not require further nursing assessment beyond providing comfort measures such as lozenges or warm saltwater gargles.
Choice C Reason:
Abdominal distention is a concerning symptom that requires further nursing assessment. It can indicate complications such as perforation, bleeding, or infection following the EGD. Perforation of the gastrointestinal tract is a rare but serious complication that can lead to peritonitis and sepsis if not promptly addressed. Therefore, any signs of abdominal distention should be reported to the provider immediately for further evaluation and intervention.
Choice D Reason:
Drowsiness is a common side effect of the sedatives used during the EGD procedure. It is expected that the client may feel drowsy or sleepy for a few hours after the procedure as the sedative wears off. This symptom does not typically require further nursing assessment unless it persists for an unusually long time or is accompanied by other concerning symptoms such as difficulty breathing or altered mental status.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A Reason:
0.45% sodium chloride (half-normal saline) is an appropriate solution for treating hypernatremia, especially in a client who is NPO (nothing by mouth). This hypotonic solution helps to gradually reduce the serum sodium levels by providing free water to the extracellular space, which dilutes the high sodium concentration. It is essential to administer this solution slowly to avoid rapid shifts in fluid balance, which can lead to cerebral edema.
Choice B Reason:
Dextrose 5% in 0.9% sodium chloride (D5NS) is not the best choice for treating hypernatremia. While it provides some free water, the presence of 0.9% sodium chloride makes it an isotonic solution, which does not effectively lower serum sodium levels. This solution is more suitable for maintaining fluid balance rather than correcting hypernatremia.
Choice C Reason:
Lactated Ringer’s is also not appropriate for treating hypernatremia. This isotonic solution contains electrolytes, including sodium, which can exacerbate hypernatremia rather than correct it. Lactated Ringer’s is typically used for fluid resuscitation and electrolyte replacement in other clinical scenarios.
Choice D Reason:
Dextrose 10% in water (D10W) is a hypertonic solution and is not suitable for treating hypernatremia. While it provides free water, the high concentration of dextrose can lead to rapid shifts in fluid balance and potential complications such as hyperglycemia. This solution is generally used for providing calories and preventing hypoglycemia in specific clinical situations.
Correct Answer is A
Explanation
Choice A Reason:
Activating the hospital’s emergency or rapid response system is the most appropriate first action in this scenario. The client is exhibiting signs of a potentially life-threatening condition, such as airway obstruction or severe swelling that could compromise breathing. Immediate intervention by a rapid response team can provide the necessary advanced airway management and other critical care measures to stabilize the patient. This action prioritizes the client’s airway, breathing, and circulation, which are the fundamental aspects of emergency care.
Choice B Reason:
Placing a heart monitor on the client and observing for dysrhythmias is important but not the immediate priority in this situation. While monitoring the heart is crucial, the client’s airway and breathing issues take precedence. Addressing the airway obstruction and ensuring adequate breathing should be the first step before focusing on cardiac monitoring.
Choice C Reason:
Asking the charge nurse to come see the client immediately is a reasonable action, but it may delay the necessary urgent intervention. The charge nurse may not have the advanced skills or equipment required to manage a severe airway obstruction. Activating the rapid response system ensures that a team of healthcare professionals with the appropriate expertise and equipment can respond quickly.
Choice D Reason:
Checking the client’s blood pressure and heart rate is a standard nursing assessment, but it is not the immediate priority in this emergency situation. The client’s difficulty breathing and stridor indicate a potential airway obstruction, which requires immediate attention. Ensuring the airway is clear and the client can breathe is more critical than checking vital signs at this moment.
Choice E Reason:
Providing a calm and assuring environment for the client is important for reducing anxiety and stress, but it does not address the immediate life-threatening issue. While maintaining a calm environment is beneficial, the nurse must first ensure that the client’s airway is secure and that they can breathe adequately. This can only be achieved by activating the rapid response system.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
