The ICU nurse provides care for a 67-year-old female patient experiencing a distributive shock. Assessment findings are indicative of decreasing cardiac output, decreased peripheral perfusion, and increased capillary permeability. The nurse identifies that the patient is in which stage of shock.
Progressive stage
Compensatory stage
Initial stage
Refractory stage
The Correct Answer is A
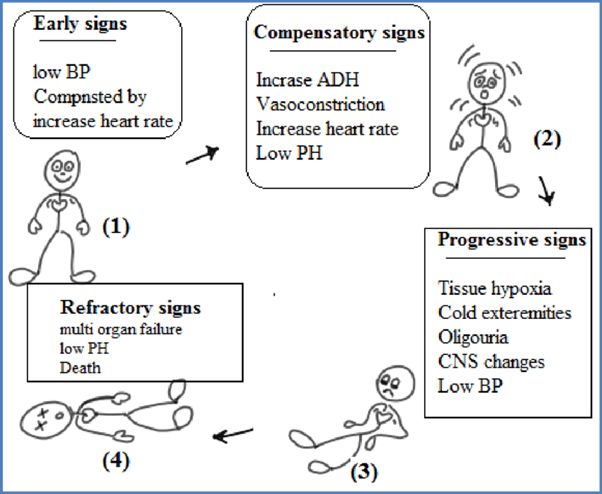
The stages of shock are commonly described as the initial, compensatory, progressive, and refractory stages. Here is an explanation of each stage and why the patient's assessment findings correspond to the progressive stage:
B. The compensatory stage in (option B) is incorrect because, In the compensatory stage, the body continues to activate compensatory mechanisms to maintain perfusion. This includes increased heart rate, peripheral vasoconstriction, and shunting of blood to vital organs. The patient's assessment findings of decreasing cardiac output, decreased peripheral perfusion, and increased capillary permeability suggest that the body's compensatory mechanisms are no longer sufficient to maintain perfusion adequately. Therefore, the patient has progressed beyond the compensatory stage.
C. The initial stage in (option C) is incorrect because, In the initial stage, there is an initial insult or injury that triggers the shock state. The body's compensatory mechanisms are activated, such as increased heart rate and vasoconstriction, to maintain blood pressure and perfusion. However, the patient's assessment findings indicate that they have progressed beyond the initial stage.
D. The refractory stage in (option D) is incorrect because The refractory stage represents a severe and irreversible state of shock where vital organs fail, and despite interventions, the patient's condition does not improve. The patient's assessment findings do not suggest the refractory stage, as there is still potential for intervention and management.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","B","D","E"]
Explanation
These manifestations occur as compensatory mechanisms in response to decreased blood volume and compromised tissue perfusion. The body attempts to compensate for the inadequate circulating volume by increasing heart rate (A) and respiratory rate (B) to enhance oxygen delivery.
D. The decreased systolic blood pressure (D) is a result of decreased cardiac output and vasoconstriction in an attempt to maintain perfusion to vital organs.
E. The decreased urine output (E) is a result of decreased renal perfusion due to decreased blood volume.
C. Decreased pulse rate in (option C) is incorrect because it is not typically seen in the compensatory stage of hypovolemic shock. The body tries to increase heart rate to maintain cardiac output and compensate for the decreased blood volume.
F. Bilateral crackles in (option F) is incorrect because the lung bases are more commonly associated with conditions such as pulmonary edema or fluid overload, rather than the compensatory stage of hypovolemic shock.
It's important to note that the manifestations of shock can vary depending on individual patient factors and the underlying cause of shock. Therefore, a comprehensive assessment and clinical judgment are necessary to fully evaluate the patient's condition.
Correct Answer is A
Explanation
The increased respiratory rate and pulse rate can be indicators of physiological changes or potential complications in the patient's condition. These changes may suggest alterations in tissue perfusion or other underlying issues that require further assessment.
Assessing the patient's tissue perfusion includes evaluating additional vital signs, such as blood pressure, oxygen saturation, and capillary refill time. Assessing skin color, temperature, and moisture, as well as peripheral pulses, can also provide important information regarding tissue perfusion.
B. Pain medication (option B) is incorrect because the increased respiratory and pulse rates could also indicate other factors that require assessment before administering pain medication.
C. Documenting the findings in the patient's chart (option C) is incorrect because it should not be the primary action at this point. Assessing the patient's condition and determining appropriate interventions take priority.
D. Increasing the rate of the patient's IV infusion (option D) is incorrect because may not be the most appropriate action without further assessment. The patient's increased respiratory and pulse rates may not necessarily be related to hydration status, and it is important to assess the patient comprehensively before making changes to the IV infusion rate.
Therefore, the best action by the nurse in this situation is to further assess the patient's tissue perfusion to gather more information and determine the appropriate course of action.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
