The nurse knows the fecal output will be more solid from a stoma created from which area of the bowel?
transverse colon
ascending colon
Ileum
sigmoid colon
The Correct Answer is D
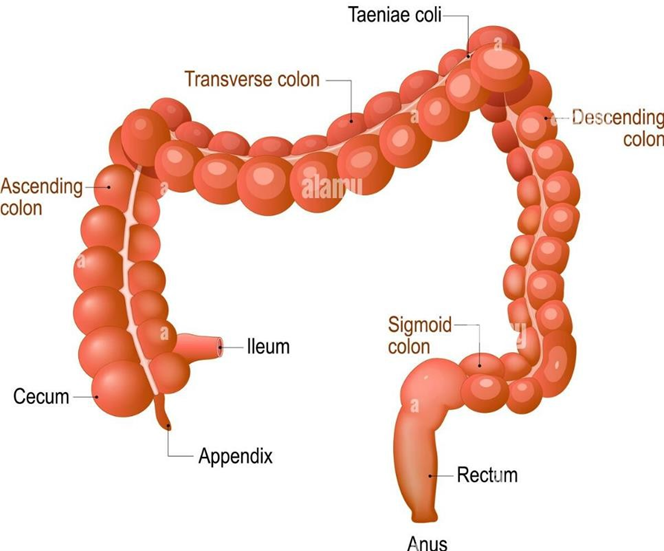
D. The sigmoid colon is the last part of the large intestine before the rectum. It functions to store fecal material and absorb water and electrolytes. Fecal material passing through the sigmoid colon tends to become more solid as water is absorbed, resulting in a more formed stool compared to other parts of the colon.
A. The transverse colon is located in the upper abdomen and is responsible for further absorption of water and electrolytes from the stool. Fecal material passing through the transverse colon tends to become more solid as water is absorbed, but it may not be as solid as stool from the descending colon or sigmoid colon.
B. The ascending colon is where stool is in a more liquid form as it moves up from the cecum. It undergoes further absorption of water and electrolytes as it travels through the colon, but it typically does not produce solid fecal output.
C. The ileum is the final portion of the small intestine and connects to the large intestine (colon). Stool passing through the ileum is still in a relatively liquid state as it contains undigested food particles, bile salts, and digestive enzymes. The primary function of the ileum is absorption of nutrients rather than water reabsorption, so fecal output from an ileostomy is usually more liquid.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
C. Assisting the client in slowed breathing techniques is the most appropriate initial intervention for a client experiencing hyperventilation due to acute psychological stress. Slowed breathing techniques, such as pursed-lip breathing or diaphragmatic breathing, can help normalize respiratory rate and depth, thereby correcting the respiratory alkalosis. Encouraging the client to breathe slowly and deeply can help reduce the respiratory rate and restore a more balanced acid-base status.
A. Administering a sedative may not be the initial intervention for a client experiencing hyperventilation due to acute psychological stress. Sedatives can depress the respiratory drive further and may exacerbate respiratory alkalosis. Additionally, administering sedatives should be based on a comprehensive assessment and medical prescription, rather than as a first-line intervention for hyperventilation.
B. While hyperventilation can sometimes lead to symptoms resembling seizure activity (such as muscle twitching or numbness), assessing for seizure activity is not typically the initial intervention for respiratory alkalosis. In the context of acute psychological stress causing hyperventilation, addressing the hyperventilation itself is the priority.
D. While monitoring vital signs, including blood pressure, is important in assessing the client's overall condition, it is not the initial intervention specifically for addressing respiratory alkalosis due to hyperventilation. The priority in this situation is to address the hyperventilation itself through appropriate breathing techniques.
Correct Answer is A
Explanation
A. Isotonic solutions have a similar osmolarity to that of blood plasma, meaning they exert the same osmotic pressure as blood. This equilibrium prevents the movement of water across cell membranes, thereby maintaining cell volume and preventing cellular dehydration or swelling. Examples of isotonic solutions commonly used for intravenous fluid replacement include 0.9% saline (normal saline) and lactated Ringer's solution.
B. Hypotonic solutions have a lower osmolarity than blood plasma, meaning they exert less osmotic pressure than blood. When administered, hypotonic solutions cause water to move into cells, leading to cellular swelling. While hypotonic solutions can help hydrate cells and replenish intracellular fluid, they are not typically used for rapid volume replacement because they can exacerbate extracellular fluid deficits and cause complications such as cerebral edema or cardiovascular collapse.
C. Hypertonic solutions have a higher osmolarity than blood plasma, meaning they exert greater osmotic pressure than blood. When administered, hypertonic solutions cause water to move out of cells, leading to cellular shrinkage. Hypertonic solutions are often used to expand intravascular volume in cases of severe hypovolemia or shock, as they rapidly increase blood osmolarity and draw fluid from the interstitial space into the bloodstream. Examples of hypertonic solutions include 3% saline and 5% dextrose in 0.9% saline.
D. Hyperosmotic solutions have an elevated osmolarity compared to blood plasma, indicating a higher concentration of solutes. These solutions exert osmotic pressure that draws water out of cells, leading to cellular dehydration. While hyperosmotic solutions are not commonly used for rapid volume replacement due to their pot
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
