In caring for the premature infant, the nurse must continually assess hydration status. Parameters to assess would include all of the following except:
Select one:
Daily weight.
Consistency of stool.
Volume of urine output.
Blood pH.
The Correct Answer is D
Choice A Reason: Daily weight. This is an incorrect answer that indicates a valid parameter to assess hydration status. Daily weight is a measure of the body mass that can reflect changes in fluid balance. Daily weight can help detect fluid loss or gain in premature infants, who are more prone to dehydration or overhydration due to immature renal function and high insensible water loss.
Choice B Reason: Consistency of stool. This is an incorrect answer that indicates a valid parameter to assess hydration status. Consistency of stool is a measure of the texture and form of feces that can reflect changes in fluid intake and absorption. Consistency of stool can help identify diarrhea or constipation in premature infants, who are more susceptible to gastrointestinal problems such as necrotizing enterocolitis or feeding intolerance.
Choice C Reason: Volume of urine output. This is an incorrect answer that indicates a valid parameter to assess hydration status. Volume of urine output is a measure of the amount of urine produced and excreted by the kidneys that can reflect changes in fluid balance and renal function. Volume of urine output can help monitor hydration status and kidney function in premature infants, who are more vulnerable to fluid overload or deficit and renal impairment.
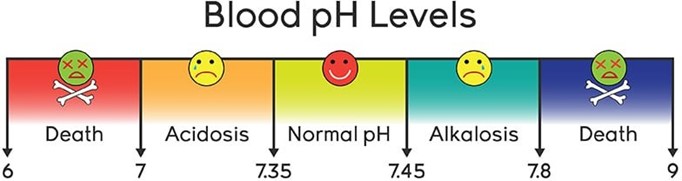
Choice D Reason: Blood pH. This is because blood pH is a measure of the acidity or alkalinity of the blood, which reflects the balance between carbon dioxide and bicarbonate in the body. Blood pH is not a direct indicator of hydration status, which refers to the amount of water and electrolytes in the body. Hydration status can affect blood pH, but blood pH can also be influenced by other factors such as respiratory or metabolic disorders.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason: Homans' sign. This is an incorrect answer that refers to a different sign that is not related to pregnancy. Homans' sign is a sign of deep vein thrombosis (DVT) that occurs when there is pain or discomfort in the calf or popliteal region when the foot is dorsiflexed. Homans' sign can be elicited by passive or active movement of the foot, but it is not a reliable or specific indicator of DVT.
Choice B Reason: Chadwick's sign. This is an incorrect answer that refers to a different sign of pregnancy that affects the color of the cervix, not the texture. Chadwick's sign is a sign of pregnancy that refers to the bluish or purplish discoloration of the cervix, vagina, and vulva due to increased blood flow and congestion. Chadwick's sign can be observed by visual inspection of the cervix during the first prenatal visit, usually around 6 to 8 weeks of gestation.
Choice C Reason: Goodell's sign. This is because Goodell's sign is a sign of pregnancy that refers to the softening of the cervix due to increased vascularity and edema. Goodell's sign can be detected by digital examination of the cervix during the first prenatal visit, usually around 6 to 8 weeks of gestation.
Choice D Reason: McDonald's sign. This is an incorrect answer that refers to a different sign of pregnancy that involves the angle of the uterus, not the cervix. McDonald's sign is a sign of pregnancy that refers to the ease of flexing the body of the uterus against the cervix, which creates an angle of 90 degrees or less. McDonald's sign can be assessed by bimanual examination of the uterus during the first prenatal visit, usually around 7 to 8 weeks of gestation.
Correct Answer is B
Explanation
Choice A Reason: Vascular spider veins. This is an incorrect answer that refers to a different skin change that occurs during pregnancy, which affects the blood vessels, not the pigment. Vascular spider veins are small red or purple clusters of blood vessels that appear on the skin, especially on the face, neck, chest, or legs. Vascular spider veins are caused by increased blood volume and hormonal changes, which dilate and rupture the capillaries. Vascular spider veins are harmless and usually disappear after delivery.
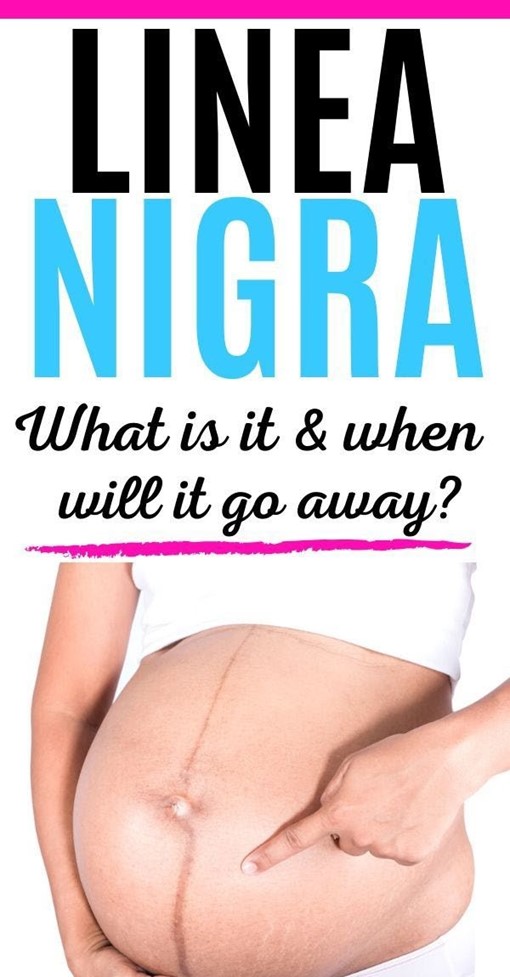
Choice B Reason: Linea nigra. This is because linea nigra is a term that refers to a darkened vertical line that appears on the abdomen during pregnancy, which runs from the umbilicus to the pubis. Linea nigra is caused by increased production of melanin, which is a pigment that gives color to the skin and hair. Linea nigra is more common and noticeable in women with darker skin tones, and it usually fades after delivery.
Choice C Reason: Melasma. This is an incorrect answer that refers to a different skin change that occurs during pregnancy, which affects the pigment, but not in a linear patern. Melasma is a term that refers to patches of brown or gray-brown discoloration that appear on the face, especially on the forehead, cheeks, nose, or upper lip. Melasma is also caused by increased production of melanin, but it is influenced by sun exposure and genetic factors. Melasma is also known as chloasma or the mask of pregnancy, and it may persist after delivery.
Choice D Reason: Striae gravidarum. This is an incorrect answer that refers to a different skin change that occurs during pregnancy, which affects the connective tissue, not the pigment. Striae gravidarum are stretch marks that appear on the skin, especially on the abdomen, breasts, hips, or thighs. Striae gravidarum are caused by rapid growth and stretching of the skin, which damage the collagen and elastin fibers. Striae gravidarum are initially red or purple, but they fade to white or silver after delivery.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
