Which of the following would the nurse include in the plan of care for a newborn receiving phototherapy? Select one:
Applying Vaseline or lotion to newborn to maximize light absorption.
Reducing the amount of fluid intake to 8 ounces daily.
Keeping the newborn in the supine position.
Feeding every 3 hours to maximize intake of fluids and output.
The Correct Answer is D
Choice A Reason: Applying Vaseline or lotion to newborn to maximize light absorption. This is an incorrect answer that indicates a contraindicated and harmful intervention that can interfere with phototherapy. Applying Vaseline or lotion to newborn can create a barrier or a reflective surface that can reduce the exposure and penetration of light to the skin, which can decrease the efficacy of phototherapy. Applying Vaseline or lotion to newborn can also cause skin irritation, infection, or burns, as it can trap heat and moisture under the light source.
Choice B Reason: Reducing the amount of fluid intake to 8 ounces daily. This is an incorrect answer that suggests a detrimental and dangerous intervention that can impair phototherapy. Reducing the amount of fluid intake to 8 ounces daily can cause dehydration, hypoglycemia, or electrolyte imbalance in newborns, which can worsen jaundice and increase the risk of complications such as kernicterus (brain damage due to high bilirubin levels). Reducing the amount of fluid intake to 8 ounces daily can also decrease the excretion of bilirubin through urine or stool, which can counteract the effect of phototherapy.
Choice C Reason: Keeping the newborn in the supine position. This is an incorrect answer that implies an incomplete and inadequate intervention that can limit phototherapy. Keeping the newborn in the supine position is a nursing action that involves placing the newborn on their back, which can expose their anterior body surface to light.
However, keeping the newborn in the supine position alone is not sufficient for phototherapy, as it does not expose their posterior body surface to light. The nurse should also reposition the newborn frequently to expose different body parts to light, such as their sides or abdomen.
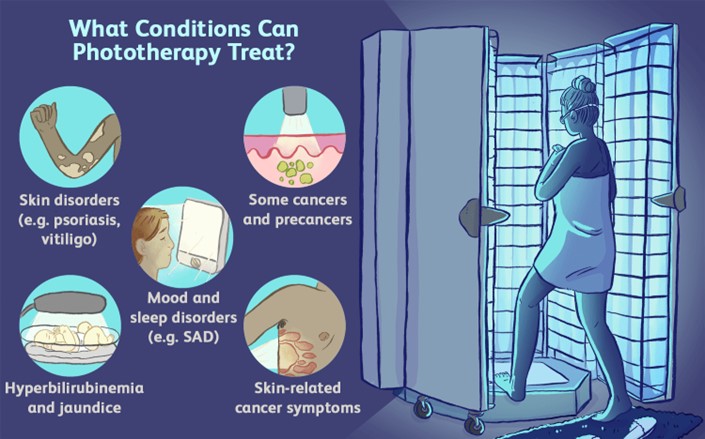
Choice D Reason: Feeding every 3 hours to maximize intake of fluids and output. This is because feeding every 3 hours is a nursing intervention that can enhance the effectiveness and safety of phototherapy, which is a treatment that uses blue or white light to reduce the level of bilirubin in the blood. Bilirubin is a yellow pigment that is produced when red blood cells are broken down, which can cause jaundice (yellowish discoloration of the skin and mucous membranes) if it accumulates in excess. Phototherapy works by converting bilirubin into a water-soluble form that can be excreted through urine or stool. Feeding every 3 hours can increase the intake of fluids and calories, which can promote hydration, nutrition, and elimination of bilirubin.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
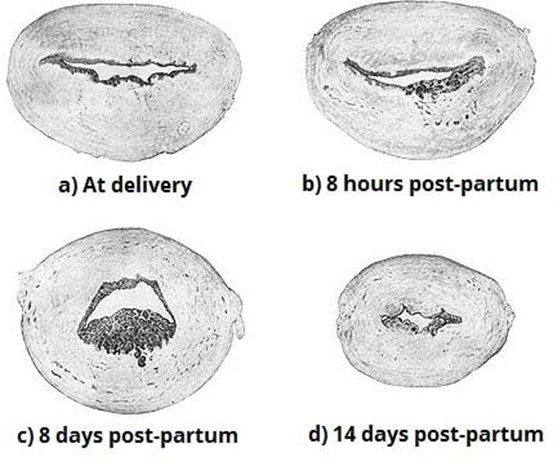
Choice A Reason: Inspecting the placenta after delivery for intactness. This is because inspecting the placenta after delivery for intactness is a nursing intervention that can prevent late postpartum hemorrhage, which is excessive bleeding from the uterus or genital tract that occurs more than 24 hours but less than 12 weeks after delivery. Late postpartum hemorrhage can be caused by retained placental fragments, subinvolution of the uterus, infection, or coagulation disorders. Inspecting the placenta after delivery for intactness can help identify and remove any retained placental fragments that may interfere with uterine contraction and involution, which are essential for hemostasis.
Choice B Reason: Manually removing the placenta at delivery. This is an incorrect answer that indicates an inappropriate and risky intervention that can cause late postpartum hemorrhage. Manually removing the placenta at delivery is a procedure that involves inserting a hand into the uterus and detaching the placenta from the uterine wall. Manually removing the placenta at delivery is indicated only for a retained or adherent placenta that does not separate spontaneously or with gentle traction within 30 minutes after delivery. Manually removing the placenta at delivery can cause trauma, infection, or incomplete removal of the placenta, which can increase the risk of late postpartum hemorrhage.
Choice C Reason: Administering broad-spectrum antibiotics prophylactically. This is an incorrect answer that suggests an unnecessary and ineffective intervention that can prevent late postpartum hemorrhage. Administering broad- spectrum antibiotics prophylactically is a pharmacological intervention that involves giving antibiotics to prevent or treat infection. Administering broad-spectrum antibiotics prophylactically is indicated for women with risk factors or signs of infection during or after delivery, such as prolonged rupture of membranes, chorioamnionitis, fever, or foul- smelling lochia. Administering broad-spectrum antibiotics prophylactically may reduce the risk of infection-related late postpartum hemorrhage, but it does not address other causes of late postpartum hemorrhage such as retained placental fragments or subinvolution of the uterus.
Choice D Reason: Applying traction on the umbilical cord to speed up separation of the placenta. This is an incorrect answer that refers to a different intervention that can prevent early postpartum hemorrhage, not late postpartum hemorrhage. Applying traction on the umbilical cord to speed up separation of the placenta is a technique that involves pulling on the umbilical cord while applying counter pressure on the uterus to facilitate placental expulsion. Applying traction on the umbilical cord to speed up separation of the placenta is indicated for active management of the third stage of labor, which can prevent early postpartum hemorrhage, which is excessive bleeding from the uterus or genital tract that occurs within 24 hours after delivery. Early postpartum hemorrhage can be caused by uterine atony, retained placenta, lacerations, or coagulation disorders.
Correct Answer is A
Explanation
Choice A Reason: Provide compassionate and accurate information throughout the process and support them to make their own decisions. This is a therapeutic strategy that demonstrates empathy, honesty, and advocacy for the couple. It also helps them understand their options, risks, benefits, and alternatives, and encourages them to participate in their care.
Choice B Reason: Inquire about the names they have chosen for their baby to get their mind off their stress. This is a non-therapeutic strategy that avoids addressing the couple's concerns, minimizes their feelings, and may create false hope or unrealistic expectations.
Choice C Reason: Express sympathy and provide directive advice to the couple about what they should do. This is a non-therapeutic strategy that shows pity, imposes personal values, and undermines the couple's self-determination.
Choice D Reason: Refer them to a marriage counselor in the same building to help them with the decisions. This is a non-therapeutic strategy that implies that the couple has marital problems, shifts responsibility, and may create resentment or resistance.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
