Why is it important for the nurse to assess the bladder regularly and encourage the laboring client to void every 2 hours?
Select one:
Frequent voiding encourages sphincter control.
A full bladder impedes oxygen flow to the fetus.
Frequent voiding prevents bruising of the bladder.
A full bladder can impede fetal descent.
The Correct Answer is D
Choice A Reason: Frequent voiding encourages sphincter control. This is an incorrect statement that has no relevance to labor and delivery. Sphincter control refers to the ability to contract and relax the muscles that control urination and defecation. It is not affected by frequent voiding.
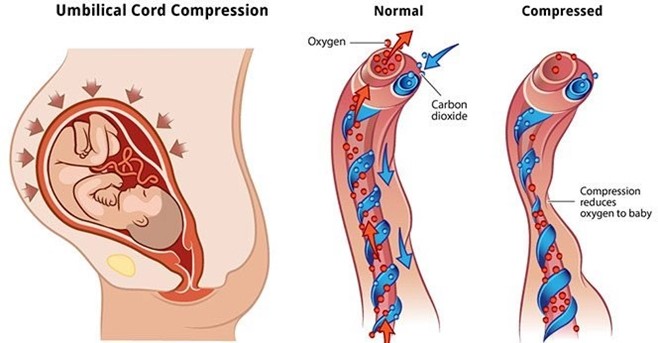
Choice B Reason: A full bladder impedes oxygen flow to the fetus. This is an incorrect statement that confuses a full bladder with a prolapsed cord. A prolapsed cord is a condition where the umbilical cord slips through the cervix before the baby and becomes compressed by the fetal head, which can reduce oxygen flow to the fetus. A full bladder does not affect oxygen flow to the fetus.
Choice C Reason: Frequent voiding prevents bruising of the bladder. This is an incorrect statement that exaggerates the effect of a full bladder on the bladder wall. A full bladder may cause some pressure or discomfort on the bladder, but it does not cause bruising or damage.
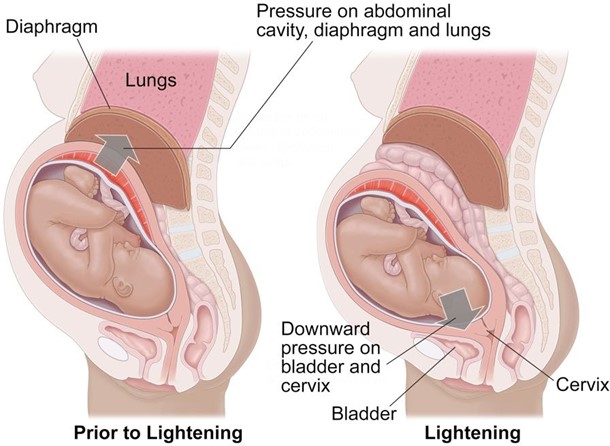
Choice D Reason: A full bladder can impede fetal descent. This is a correct statement that explains why it is important for the nurse to assess the bladder regularly and encourage the laboring client to void every 2 hours.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason: Late decelerations. This is an incorrect answer that refers to a different type of fetal heart rate patern that indicates uteroplacental insufficiency, which can reduce blood flow and oxygen delivery to the fetus. Late decelerations are characterized by gradual decreases in fetal heart rate that begin after the peak of uterine contractions and return to baseline after the end of contractions. Amnioinfusion is not effective for late decelerations, as it does not address the underlying cause of uteroplacental insufficiency, which may be due to maternal hypertension, diabetes, preeclampsia, or placental abruption.
Choice B Reason: Moderate decelerations. This is an incorrect answer that refers to a non-existent type of fetal heart rate patern, as there is no such term as moderate decelerations. The term moderate refers to the category of fetal heart rate variability, which is a measure of the fluctuations in fetal heart rate around the baseline. Moderate variability indicates normal fetal oxygenation and well-being, while absent or minimal variability indicates fetal hypoxia or distress.
Choice C Reason: Variable decelerations. This is because variable decelerations are a type of fetal heart rate patern that indicates cord compression, which can reduce blood flow and oxygen delivery to the fetus. Variable decelerations are characterized by abrupt decreases in fetal heart rate that vary in onset, depth, and duration, and do not have a consistent relationship with uterine contractions. Amnioinfusion is a procedure that involves infusing saline or lactated Ringer's solution into the amniotic cavity through a transcervical catheter, which can relieve cord compression by increasing the volume of amniotic fluid and cushioning the cord. Amnioinfusion can improve fetal oxygenation and reduce variable decelerations.
Choice D Reason: Early decelerations. This is an incorrect answer that refers to a different type of fetal heart rate patern that indicates head compression, which can stimulate the vagus nerve and slow down the fetal heart rate. Early decelerations are characterized by gradual decreases in fetal heart rate that begin with the onset of uterine contractions and return to baseline with the end of contractions. Early decelerations are benign and do not require intervention, as they reflect normal fetal head descent and progress of labor. Amnioinfusion is not indicated for early decelerations, as it does not affect head compression or vagal stimulation.
Correct Answer is C
Explanation
Choice A Reason: Continuing to monitor and document fetal heart rate. This is an inadequate response that does not address the urgency of the situation or intervene to prevent fetal distress or demise.
Choice B Reason: Changing the mother's position to left lateral and giving oxygen by nasal cannula. This is a partial response that may improve maternal-fetal blood flow and oxygenation, but it does not resolve the cord compression or facilitate delivery.
Choice C Reason: With a sterile glove, maintaining pressure to lift the presenting part and emergently notifying the provider for a STAT C-section. This is an appropriate response that aims to reduce the cord compression by elevating the fetal head away from the cord and prepare for an immediate cesarean delivery.
Choice D Reason: Bolusing the patient with 1000cc lactated ringers. This is an irrelevant response that does not address the cause of the problem or improve fetal outcome.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
