Ati adult med Surg nurs 4292 exam
Ati adult med Surg nurs 4292 exam
Total Questions : 78
Showing 10 questions Sign up for moreA nurse is caring for a client who has a T-4 spinal cord injury. Which of the following findings should the nurse identify as a potential cause for autonomic dysreflexia?
Explanation
Choice A reason: A distended bladder is a common cause of autonomic dysreflexia. It can trigger an exaggerated response from the autonomic nervous system, leading to a rapid increase in blood pressure. This is because the full bladder sends signals to the spinal cord, which then attempts to send signals to the brain. However, due to the injury, these signals cannot pass through, resulting in a reflex that increases blood pressure.
Choice B reason: While a severe headache is a symptom of autonomic dysreflexia, it is not a cause. The headache results from the body's response to a triggering stimulus, such as a distended bladder, which leads to the high blood pressure characteristic of autonomic dysreflexia.
Choice C reason: Nasal congestion is not typically a cause of autonomic dysreflexia. The condition is usually triggered by a noxious stimulus below the level of the spinal cord injury, such as a full bladder or bowel, skin irritation, or other types of physical discomfort.
Choice D reason: Elevated blood pressure is a symptom, not a cause, of autonomic dysreflexia. The condition itself causes a sudden spike in blood pressure due to an uncontrolled reflex sympathetic discharge in response to a triggering stimulus below the level of the injury.
A nurse is planning care for a client who is receiving enteral feedings through a nasogastric (NG) tube. Which of the following actions should the nurse plan to take first?
Explanation
Choice A reason:Labeling the feeding bag with the date and time is important for tracking, but it is not the first action to take. The priority is to ensure that the NG tube is correctly placed and the stomach contents can be aspirated to verify placement before administering the feeding.
Choice B reason:Aspirating the client's stomach contents is the first action the nurse should take. This is to confirm the correct placement of the NG tube to prevent complications such as aspiration pneumonia. It is a critical step before starting any enteral feeding.
Choice C reason: Hanging the feeding bag 30 cm (12 inches) above the client is necessary for gravity feeding, but it comes after verifying the NG tube placement through aspiration of stomach contents.
Choice D reason:Warming the feeding to room temperature is a comfort measure and helps to prevent gastrointestinal discomfort. However, it is not the first action to take. The priority is to check the tube placement.
A client with a history of angina is being admitted to the emergency department with a suspected myocardial infarction (MI). Which of the following findings will help the nurse distinguish stable angina from an MI?
Explanation
Choice A reason: Myocardial infarction (MI) is not limited to occurrences with exertion. While stable angina typically occurs during physical activity or emotional stress, MI can happen at any time, even at rest. The underlying cause of an MI is the complete blockage of blood supply to a part of the heart muscle, usually due to a blood clot in a coronary artery. This blockage can lead to the death of heart muscle tissue, a condition that requires immediate medical attention.
Choice B reason: Stable angina does not typically last for more than 30 minutes. It is characterized by chest pain or discomfort that occurs predictably with exertion or emotional stress and is relieved within minutes by rest or nitroglycerin. In contrast, the pain from an MI is more prolonged and severe, and it is not relieved by rest or nitroglycerin. If chest discomfort lasts longer than 15 minutes and is not alleviated by rest or nitroglycerin, it is a warning sign that the individual may be experiencing an MI.
Choice C reason: This is the distinguishing feature between stable angina and an MI. Stable angina is usually relieved within 3-5 minutes by rest or nitroglycerin, which helps to dilate the coronary arteries and improve blood flow to the heart muscle. Nitroglycerin is ineffective in relieving the symptoms of an MI because the problem is not just reduced blood flow but a complete blockage that nitroglycerin cannot overcome.
Choice D reason: The pain associated with an MI typically lasts for more than 15 minutes and can be quite severe. Unlike stable angina, the pain of an MI is not relieved by rest or nitroglycerin. The duration and severity of the pain, along with other symptoms such as shortness of breath, sweating, nausea, or lightheadedness, help differentiate an MI from stable angina.

A nurse is obtaining a health history for a client with chronic pancreatitis. Which of the following indicates the primary cause of the client's condition?
Explanation
Choice A reason: Weight gain is not typically a direct cause of chronic pancreatitis. While obesity can be a risk factor for developing pancreatitis, it is not considered a primary cause.
Choice B reason: The use of alcohol is the most common cause of chronic pancreatitis. Long-term alcohol misuse can lead to the development of chronic pancreatitis, accounting for about 70% of cases³.
Choice C reason: Abdominal pain that is relieved with food or antacids is more indicative of conditions like peptic ulcers rather than chronic pancreatitis.
Choice D reason:Exposure to occupational chemicals has not been established as a primary cause of chronic pancreatitis. While certain toxins can affect the pancreas, they are not a common cause of chronic pancreatitis.
A nurse is caring for a client who has valvular heart disease and is at risk for developing left-sided heart failure. Which of the following manifestations should alert the nurse that the client is developing this condition?
Explanation
Choice A reason: Anorexia, or loss of appetite, is not typically a direct manifestation of left-sided heart failure. While it can be associated with many medical conditions and may occur in the context of heart failure due to overall decreased well-being, it is not a specific indicator of left-sided heart failure.
Choice B reason: Weight gain can be associated with heart failure, but it is more commonly a sign of right-sided heart failure, where fluid accumulates in the body tissues, causing swelling and weight increase. In left-sided heart failure, weight gain is not as prominent because the primary issue is the backup of blood into the lungs, not fluid retention in the tissues.
Choice C reason: A distended abdomen can occur in heart failure due to fluid accumulation; however, it is more characteristic of right-sided heart failure, where the failure of the right ventricle leads to systemic congestion, including the abdominal area. In left-sided heart failure, the primary effect is on the lungs, not the abdomen.
Choice D reason: Dyspnea, or difficulty breathing, is a hallmark symptom of left-sided heart failure. It occurs due to the backup of blood in the pulmonary circulation, which leads to pulmonary congestion and reduced oxygen exchange. Patients may experience shortness of breath, especially during exertion or when lying flat (orthopnea), and may wake up at night with shortness of breath (paroxysmal nocturnal dyspnea).
Left-sided heart failure, often caused by conditions like valvular heart disease, leads to a decrease in the heart’s ability to pump blood effectively. This results in a buildup of pressure in the lungs, manifesting as dyspnea, which is an important symptom for nurses and other healthcare providers to recognize and manage promptly.
A nurse is caring for a client who has just developed a pulmonary embolism. Which of the following medications should the nurse anticipate administering?
Explanation
Choice A reason: Atropine is not typically used for the treatment of pulmonary embolism. It is an anticholinergic drug that is primarily used to treat bradycardia (slow heart rate) and as part of the management of organophosphate poisoning. It does not have a role in the management of pulmonary embolism, which requires anticoagulation to prevent further clot formation.
Choice B reason: Furosemide is a loop diuretic commonly used to treat fluid overload conditions such as heart failure or edema. While it can help relieve symptoms associated with fluid accumulation, it does not treat the underlying cause of a pulmonary embolism, which is a blood clot in the pulmonary arteries.
Choice C reason: Heparin is an anticoagulant medication that is commonly used in the initial treatment of pulmonary embolism. It works by preventing the formation of new blood clots and stopping existing clots from getting bigger. Heparin is often administered intravenously or subcutaneously and is a key component in the management of pulmonary embolism.
Choice D reason: Dexamethasone is a corticosteroid that is used to reduce inflammation in various conditions, such as allergic reactions, asthma, and certain types of arthritis. It is not used as a primary treatment for pulmonary embolism, as it does not have anticoagulant properties.
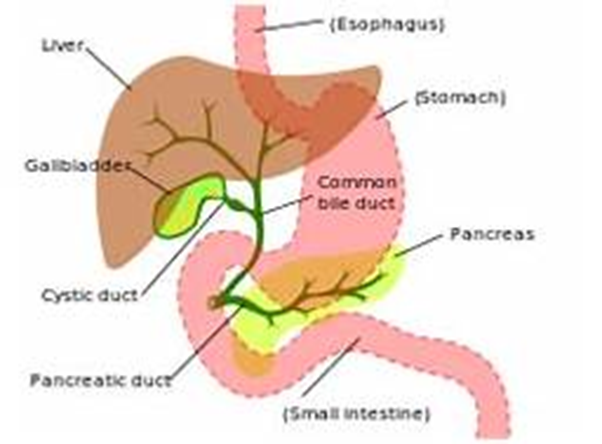
A nurse is assessing a client who has an obstruction of the common bile duct resulting from chronic cholecystitis. Which of the following findings should the nurse expect?
Explanation
Choice A reason: Tenderness in the left upper abdomen is not typically associated with an obstruction of the common bile duct. This symptom is more commonly related to conditions affecting the stomach, pancreas, or spleen. The common bile duct is in the right upper quadrant of the abdomen, and tenderness in this area might be expected with its obstruction.
Choice B reason: Ecchymosis of the extremities is not a common finding in common bile duct obstruction. Ecchymosis, or bruising, is usually due to trauma, blood disorders, or other causes of fragile blood vessels and is not related to bile duct issues.
Choice C reason: Pale-colored urine is the opposite of what might be expected with common bile duct obstruction. Typically, the urine may become dark due to increased bilirubin levels that are excreted by the kidneys when the bile duct is obstructed.
Choice D reason: Fatty stools, or steatorrhea, are a classic finding in common bile duct obstruction. When bile flow is blocked, fats are not properly digested and absorbed, leading to stools that are bulky, greasy, and often have a foul odor. This occurs because bile is necessary for the emulsification and absorption of dietary fats in the intestine.
A client is admitted to the emergency room with renal calculi. Upon assessment, which of the following findings should the nurse expect?
Explanation
Choice A reason: Bradycardia, which is a slower than normal heart rate, is not a common finding associated with renal calculi. Renal calculi, or kidney stones, typically cause symptoms related to the urinary system rather than directly affecting the heart rate.
Choice B reason: Bradypnea, or abnormally slow breathing, is also not a typical symptom of renal calculi. Patients with kidney stones may experience changes in urination patterns, such as frequency or urgency, but not typically changes in respiratory rate.
Choice C reason: Severe pain is indeed the most common symptom associated with renal calculi. This pain, known as renal colic, is often sudden in onset, very severe, and may radiate from the back down to the lower abdomen or groin. The pain is caused by the stone moving into the ureter and causing a blockage, which leads to increased pressure and stretching of the kidney or ureter. Renal calculi can cause a range of symptoms, with severe pain being the most prominent and often the first symptom that leads individuals to seek medical care. The pain is typically very intense and can be accompanied by other symptoms such as nausea, vomiting, and hematuria (blood in the urine).
Choice D reason: Nocturia, or frequent urination at night, can be a symptom of renal calculi, especially if the stones affect the bladder or cause urinary tract infections. However, the most characteristic symptom of renal calculi is severe pain, not necessarily nocturia.
A nurse is caring for a client who is receiving continuous enteral nutrition and develops refeeding syndrome. The nurse should expect which of the following laboratory findings?
Explanation
Choice A reason: Hypermagnesemia, or high levels of magnesium in the blood, is not typically associated with refeeding syndrome. Instead, refeeding syndrome can lead to hypomagnesemia, which is a low level of magnesium in the blood, due to shifts of magnesium into the cells during insulin secretion in the refeeding process.
Choice B reason: Hyponatremia, or low levels of sodium in the blood, is not a hallmark of refeeding syndrome. While fluid shifts can affect sodium levels, the key electrolyte disturbances in refeeding syndrome involve phosphorus, potassium, and magnesium.
Choice C reason: Hyperkalemia, or high levels of potassium in the blood, is not a common finding in refeeding syndrome. Similar to magnesium, potassium can shift into cells during refeeding, which can actually lead to hypokalemia, or low levels of potassium in the blood.
Choice D reason: Hypophosphatemia, or low levels of phosphorus in the blood, is the hallmark of refeeding syndrome. When a malnourished individual is refed, insulin secretion is stimulated by the increased carbohydrate intake. Insulin promotes cellular uptake of glucose, which is accompanied by phosphate, potassium, and magnesium, leading to a decrease in the serum levels of these electrolytes. Phosphorus is critical for cellular processes, and its deficiency can lead to muscle weakness, respiratory failure, hemolysis, and impaired cardiac function. During refeeding, careful monitoring of electrolytes is essential to prevent and manage refeeding syndrome. Hypophosphatemia is the most significant laboratory finding to anticipate in a patient with refeeding syndrome, and it requires prompt recognition and treatment to prevent serious complications.
The healthcare provider prescribes lactulose for a patient with hepatic encephalopathy. What will the nurse assess to determine the effectiveness of this medication?
Explanation
Choice A reason:Lactulose is used in hepatic encephalopathy primarily to lower blood ammonia levels. It works by converting ammonia in the intestines into ammonium, which is then excreted³. Therefore, a decrease in ammonia levels would indicate the effectiveness of the medication.
Choice B reason:While lactulose can relieve constipation due to its laxative effect, relief of constipation is not the primary indicator of its effectiveness in treating hepatic encephalopathy³.
Choice C reason:Decreased liver enzymes are not a direct measure of lactulose's effectiveness in hepatic encephalopathy. Liver enzymes are indicators of liver function, not ammonia levels³.
Choice D reason:Relief of abdominal pain is not a specific indicator of lactulose's effectiveness in hepatic encephalopathy. The medication's primary role is to reduce ammonia levels, not to alleviate pain³.
You just viewed 10 questions out of the 78 questions on the Ati adult med Surg nurs 4292 exam Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



