Med Surg 2
ATI Med Surg 2
Total Questions : 50
Showing 10 questions Sign up for moreThe nurse is evaluating a client who had a cardiac catheterization with a left antecubital insertion site. Which of the following pulses should the nurse palpate?
Explanation
The correct answer is: d. Brachial pulse in the right arm.
Choice A reason: Palpating the radial pulse in the right arm is not the most appropriate choice following a cardiac catheterization with a left antecubital insertion site. While it is contralateral to the insertion site, the brachial pulse is preferred over the radial pulse for assessing circulation in the arm, as it is more proximal and can provide a better indication of arterial flow from the catheterization site.
Choice B reason: The radial pulse in the left arm is the correct choice because it evaluates distal circulation in the affected limb. Since the catheterization was performed through the left antecubital fossa, it is crucial to monitor blood flow further down in the arm. Palpating the radial pulse helps detect early signs of compromised perfusion, such as diminished pulse strength. Evidence-based guidelines from clinical sources highlight the importance of distal pulse assessment post-catheterization.
Choice C reason: Palpating the brachial pulse in the left arm is also not recommended. Since the catheterization was performed on the left side, there is a risk of arterial occlusion or spasm, which could affect the accuracy of the pulse assessment in the left arm.
Choice D reason: The brachial pulse in the right arm does not provide relevant information about the left arm’s vascular status post-catheterization. Since the right arm was not affected by the procedure, its pulse does not indicate possible complications in the left arm. Clinical assessment should focus on detecting perfusion issues in the limb where the catheter was inserted. Best practices recommend prioritizing the evaluation of circulation in the affected extremity.
A nurse is receiving a transfer report for a client who has a head injury. The client has a Glasgow Coma Scale (GCS) score of 3 for eye opening, 5 for best verbal response, and 5 for best motor response. Which of the following is an appropriate conclusion based on this data?
Explanation
Choice A Reason: This is incorrect because the client's best motor response is 5, which means he can localize pain, not follow commands.
Choice B Reason: This is incorrect because the client's eye opening response is 3, which means he opens his eyes to pain, not to speech.
Choice C Reason: This is correct because the client's GCS score is 13, which indicates a severe impairment of consciousness. The GCS is a tool used to assess the level of consciousness of a person who has a head injury. The GCS score ranges from 3 to 15, with lower scores indicating lower levels of consciousness. A GCS score of 8 or less indicates coma. The client's GCS score is 3 + 5 + 5 = 13, which is above the coma threshold, but still indicates a severe impairment of consciousness. The other choices are not consistent with the client's GCS score.
Choice D Reason: This is incorrect because the client's best verbal response is 5, which means he can orient himself to person, place, and time, not that he is unable to make vocal sounds.
A nurse is helping to triage a group of clients at a mass casualty incident who were involved in an explosion at a local factory. Which of the following clients should the nurse tag to be the priority for care?
Explanation
Choice A Reason: This is incorrect because this client has signs of brain death, such as severe head injuries, low respiratory rate, and unresponsiveness. The nurse should tag this client as black, which means deceased or expectant.
Choice B Reason: This is incorrect because this client has non-life-threatening injuries, such as a simple fracture and scratches. The nurse should tag this client as green, which means minor or delayed care.
Choice C Reason: This is incorrect because this client has minor injuries and is able to walk around. The nurse should tag this client as green, which means minor or delayed care.
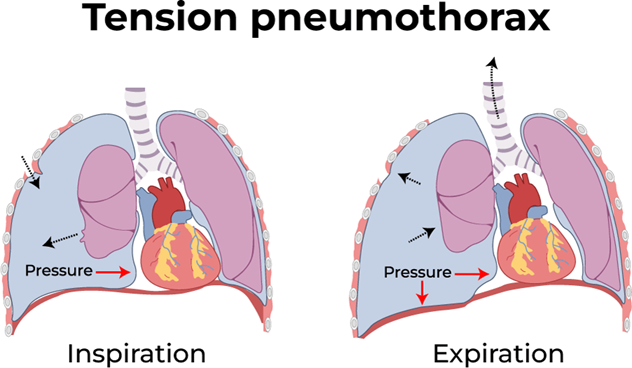
Choice D Reason: This is correct because this client has a life-threatening condition called tension pneumothorax, which requires immediate care. This client has a life-threatening condition called tension pneumothorax, which is caused by air leaking into the pleural space and compressing the lung and the heart. This can lead to respiratory failure, cardiac arrest, and death if not treated immediately. The hissing sound indicates that air is escaping from the lung through the wound. The nurse should tag this client as red, which means immediate care is needed.
A nurse is preparing to administer dabigatran to a client who has atrial fibrillation. The nurse should explain that the purpose of this medication is which of the following?
Explanation
Choice A Reason: This is incorrect because dabigatran does not affect the electrical activity of the heart or the conduction system. It does not slow down the ventricular response to the atrial impulses.
Choice B Reason: This is incorrect because dabigatran does not dissolve existing clots in the bloodstream. It only prevents new clots from forming.
Choice C Reason: This is correct because dabigatran reduces the risk of stroke in clients who have atrial fibrillation by preventing clot formation and reducing blood viscosity. Dabigatran is an anticoagulant medication that prevents the formation of blood clots in the heart and blood vessels. Atrial fibrillation is a condition where the atria beat irregularly and rapidly, which can cause blood to pool and clot in the heart chambers. These clots can travel to the brain and cause a stroke. Dabigatran reduces the risk of stroke by preventing clot formation and reducing blood viscosity.
Choice D Reason: This is incorrect because dabigatran does not restore normal sinus rhythm in clients who have atrial fibrillation. It does not affect the heart rate or rhythm.
A nurse is caring for a client who has a serum potassium level of 5.5 mEq/L. The provider prescribes polystyrene sulfonate. If this medication is effective, the nurse should expect which of the following changes on the client’s ECG?
Explanation
Choice A Reason: This is incorrect because shortening of P-wave duration is not a sign of hyperkalemia or its reversal.
P-wave duration reflects the time it takes for the atria to depolarize and contract.
Choice B Reason: This is incorrect because restoration of QRS complex amplitude is not a sign of hyperkalemia or its reversal. QRS complex amplitude reflects the voltage or strength of the ventricular depolarization and contraction.
Choice C Reason: This is correct because the reduction of T-wave amplitude is a sign of hyperkalemia reversal. T-wave amplitude reflects the repolarization or recovery of the ventricles after contraction. Polystyrene sulfonate is a medication that lowers the serum potassium level by binding to it in the gastrointestinal tract and excreting it in the stool. High serum potassium level, or hyperkalemia, can cause cardiac arrhythmias and ECG changes, such as peaked T waves, prolonged PR interval, flatened P waves, widened QRS complex, and ventricular fibrillation. By lowering the serum potassium level, polystyrene sulfonate can reverse these ECG changes and normalize the cardiac rhythm.
Choice D Reason: This is incorrect because the widening of the QRS complex is a sign of hyperkalemia, not its reversal. Widening of the QRS complex reflects the delay or impairment of ventricular depolarization and contraction.

A nurse in an emergency department is caring for a client who is bleeding profusely from a deep laceration on his left lower forearm. After observing standard precautions, which of the following actions should the nurse perform first?
Explanation
Choice A Reason: This is incorrect because cleaning the wound is not a priority when the client is bleeding profusely. Cleaning the wound can also dislodge any clots that have formed and increase bleeding.
Choice B Reason: This is incorrect because applying a tourniquet is a last resort when direct pressure fails to stop bleeding. A tourniquet can cause tissue damage, nerve injury, and infection if applied incorrectly or for too long.
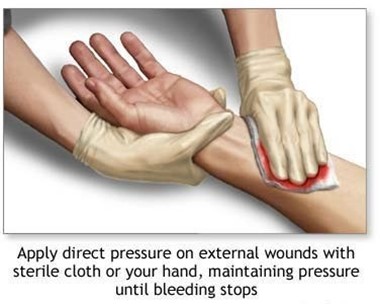
Choice C Reason: This is correct because applying direct pressure over the wound is the first and most effective action to stop bleeding from a wound. This is the first and most effective action to stop bleeding from a wound. Direct pressure compresses the blood vessels and prevents further blood loss. The nurse should use a clean cloth or dressing to cover the wound and apply firm pressure with both hands.
Choice D Reason: This is incorrect because elevating the limb and applying ice are not effective actions to stop bleeding from a wound. Elevating the limb can reduce blood flow to the injured area, but it does not compress the blood vessels or prevent blood loss. Applying ice can cause vasoconstriction, but it can also damage the skin and tissues if applied for too long.
A nurse is caring for a client who has hypertension and develops epistaxis. Which of the following actions should the nurse take? (Select all that apply.)
Explanation
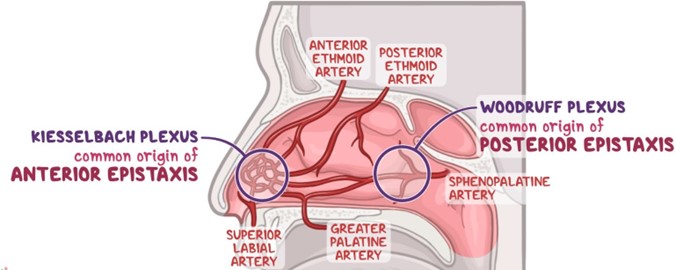
Choice A Reason: This is correct because placing ice to the bridge of the client’s nose can cause vasoconstriction and reduce blood flow to the nasal mucosa.
Choice B Reason: This is incorrect because tilting the client's head backward can cause blood to drain into the throat and increase the risk of aspiration, nausea, and vomiting.
Choice C Reason: This is correct because moving the client into high-Fowler position can lower the blood pressure in the head and neck and decrease bleeding.
Choice D reason Reason This is incorrect because instructing the client to blow his nose can dislodge any clots that have formed and worsen bleeding.
Choice E Reason: This is correct because applying pressure to the nares can compress the bleeding site and promote clotting.
A nurse is reviewing the arterial blood gas values of a client who has chronic kidney disease. Which of the following sets of values should the nurse expect?
Explanation
Choice A Reason: This is incorrect because these values indicate respiratory alkalosis, which is caused by hyperventilation or excess loss of carbon dioxide (PaCO2). Respiratory alkalosis increases the blood pH and decreases the HCO3- level.
Choice B Reason: This is incorrect because these values indicate metabolic alkalosis, which is caused by excess intake or retention of bases or loss of acids. Metabolic alkalosis increases the blood pH and the HCO3- level.
Choice C Reason: This is incorrect because these values indicate respiratory acidosis, which is caused by hypoventilation or excess retention of carbon dioxide (PaCO2). Respiratory acidosis decreases the blood pH and increases the HCO3- level.
Choice D Reason: This is correct because these values indicate metabolic acidosis, which is a common complication of chronic kidney disease. These values indicate metabolic acidosis, which is a common complication of chronic kidney disease. Metabolic acidosis occurs when the kidneys are unable to excrete excess acids or retain enough bicarbonate (HCO3-), which is a base that buffers the blood pH. As a result, the blood pH decreases and becomes more acidic. The normal range for blood pH is 7.35 to 7.45, for HCO3- is 22 to 26 mEq/L, and for PaCO2 is 35 to 45 mm Hg.
A nurse is planning a staff education session regarding biological weapons of mass destruction. Which of the following should he plan to include in the session? (Select all that apply.)
Explanation
Choice A Reason: This is correct because smallpox is a highly contagious and deadly viral disease that can be used as a biological weapon. Smallpox was eradicated in 1980, but some samples of the virus are still stored in laboratories. If released intentionally, smallpox could cause a global pandemic.
Choice B Reason: This is incorrect because hydrogen cyanide is a chemical weapon of mass destruction, not a biological one. Hydrogen cyanide is a colorless gas that interferes with cellular respiration and causes rapid death.
Choice C Reason: This is correct because botulism is a serious and potentially fatal illness caused by a toxin produced by the bacterium Clostridium botulinum. Botulism can be used as a biological weapon by contaminating food or water supplies or by aerosolizing the toxin.
Choice D Reason: This is correct because anthrax is an infection caused by the spore-forming bacterium Bacillus anthracis. Anthrax can be used as a biological weapon by releasing the spores into the air or by contaminating food or water sources.
Choice E Reason: This is incorrect because sarin is a chemical weapon of mass destruction, not a biological one. Sarin is a nerve agent that blocks the transmission of nerve impulses and causes respiratory failure and death.

A nurse is performing cardiopulmonary resuscitation (CPR) for an adult client who is unresponsive. The nurse should evaluate the client's circulation by palpating which of the following pulses?
Explanation
Choice A Reason: This is correct because the carotid pulse is the most accessible and reliable pulse to check during CPR for an adult client. The carotid pulse is the most accessible and reliable pulse to check during CPR for an adult client. The carotid pulse is located on the side of the neck, near the trachea. The nurse should use two fingers to palpate the carotid pulse for at least 5 seconds and no more than 10 seconds.
Choice B Reason: This is incorrect because the popliteal pulse is located behind the knee and is not easily palpable during CPR.
Choice C Reason: This is incorrect because the radial pulse is located on the wrist and may not be detectable during CPR due to low blood pressure or peripheral vasoconstriction.
Choice D Reason: This is incorrect because the apical pulse is located on the chest and requires a stethoscope to auscultate. The nurse should not interrupt chest compressions or ventilations to listen to the apical pulse during CPR.
You just viewed 10 questions out of the 50 questions on the ATI Med Surg 2 Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



