Med Surg Custom N235 Final Summer 2023
ATI Med Surg Custom N235 Final Summer 2023
Total Questions : 70
Showing 10 questions Sign up for moreA nurse in an emergency department is preparing to care for a client who is being brought in with multiple system trauma following a motor vehicle crash. Which of the following should the nurse identify as the priority focus of care?
Explanation
Choice A Reason: Preventing musculoskeletal disability is important, but not the priority focus of care. The nurse should first assess and manage the client's life-threatening injuries, such as airway obstruction, bleeding, shock, or brain injury.
Choice B Reason: Airway protection is the priority focus of care for a client with multiple system trauma. The nurse should ensure that the client has a patent airway and adequate ventilation, as any compromise in these areas can quickly lead to hypoxia, respiratory failure, and death.
Choice C Reason: Stabilizing cardiac arrhythmias is also important, but not the priority focus of care. The nurse should monitor the client's cardiac rhythm and treat any arrhythmias that may occur, but only after securing the airway and breathing.
Choice D Reason: Decreasing intracranial pressure is another important goal, but not the priority focus of care. The nurse should assess the client's neurological status and intervene to prevent or reduce increased intracranial pressure, such as elevating the head of the bed, maintaining normothermia, and administering osmotic diuretics. However, these measures are secondary to ensuring adequate oxygenation and perfusion.
The nurse is caring for a postoperative client who has a chest tube connected to suction and a water seal drainage system. Which of the following indicates to the nurse that the chest tube is functioning properly?
Explanation
Choice A Reason: Equal amount of fluid drainage in each collection chamber is not a sign of proper chest tube function. The amount of fluid drainage depends on the type and extent of the client's injury or surgery, and may vary from one chamber to another.
Choice B Reason:Fluctuation of the fluid level in the water seal chamber(tidaling) indicates that the chest tube is functioning properly. This fluctuation corresponds with the client's respirations and shows that air or fluid is being effectively removed from the pleural space.
Choice C Reason:Continuous bubbling within the water seal chamber: Continuous bubbling in the water seal chamber indicates an air leak, which is not normal unless the client has a pneumothorax and air is being evacuated. Otherwise, it suggests a problem with the system.
Choice D Reason: Absence of fluid in the drainage tubing is not a sign of proper chest tube function. It may indicate that the chest tube is obstructed, kinked, or clamped, or that the suction is not working properly. The nurse should assess and troubleshoot the chest tube system.
A nurse in the emergency department is caring for a client who has extensive partial and full-thickness burns of the head, neck, and chest. While planning the client's care, the nurse should identify which of the following risks as the priority for assessment and intervention?
Explanation
Choice A Reason: Infection is a serious complication of burn injuries, but not the priority risk for assessment and intervention. The nurse should monitor the client's wound healing, temperature, white blood cell count, and signs of sepsis, and administer antibiotics as prescribed. However, these measures are secondary to ensuring adequate oxygenation and ventilation.
Choice B Reason: Airway obstruction is the priority risk for assessment and intervention for a client who has burns of the head, neck, and chest. The nurse should assess the client's airway patency, respiratory rate, oxygen saturation, breath sounds, and signs of respiratory distress, such as stridor, wheezes, or cyanosis. The nurse should also provide humidified oxygen, suction secretions, elevate the head of the bed, and prepare for endotracheal intubation if needed. Airway obstruction can occur due to edema, inflammation, or inhalation injury of the upper airway, and can quickly lead to hypoxia, respiratory failure, and death.
Choice C Reason: Paralytic ileus is a potential complication of burn injuries, but not the priority risk for assessment and intervention. The nurse should assess the client's bowel sounds, abdominal distension, nausea, vomiting, and stool output, and administer fluids, electrolytes, and nutritional support as prescribed. However, these measures are secondary to ensuring adequate oxygenation and ventilation.
Choice D Reason: Fluid imbalance is another potential complication of burn injuries, but not the priority risk for assessment and intervention. The nurse should assess the client's fluid status, urine output, vital signs, weight, and serum electrolytes, and administer intravenous fluids as prescribed. However, these measures are secondary to ensuring adequate oxygenation and ventilation.
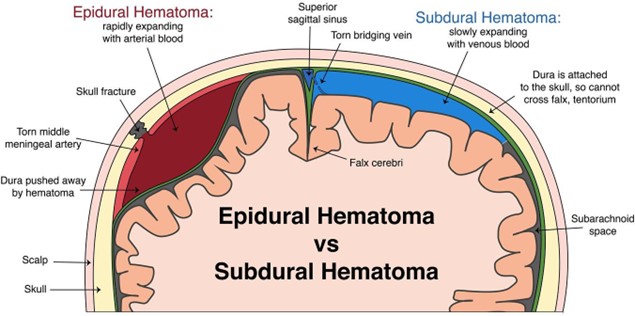
A nurse is caring for a client who had an evacuation of a subdural hematoma. Which of the following actions should the nurse take first?
Explanation
Choice A Reason: Observing for cerebrospinal fluid (CSF) leaks from the evacuation site is important, but not the first action that the nurse should take. CSF leaks can indicate a breach in the dura mater, which can increase the risk of infection and meningitis. The nurse should inspect the dressing and the nose and ears for any clear or bloody drainage, and report any findings to the provider. However, these measures are secondary to ensuring adequate oxygenation and perfusion.
Choice B Reason: The first action the nurse should take when caring for a client post-evacuation of a subdural hematoma is to check the oximeter to ensure adequate oxygenation. Maintaining proper oxygenation is a priority because hypoxia and hypercapnia can lead to cerebral vasodilation, increasing intracranial pressure (ICP) and worsening neurological outcomes.Key Concept: Always prioritize Airway, Breathing, and Circulation (ABCs) when determining the most immediate nursing intervention.
Choice C Reason: Assessing for an increase in temperature is another important action, but not the first one that the nurse should take. An increase in temperature can indicate an infection, inflammation, or damage to the hypothalamus, which can affect the thermoregulation of the body. The nurse should monitor the temperature and administer antipyretics as prescribed. However, these measures are secondary to ensuring adequate oxygenation and perfusion.
Choice D Reason:This is crucial, but oxygenation status should be checked first since low oxygen levels can worsen ICP.
A nurse is caring for a client who had an evacuation of a subdural hematoma. Which of the following actions should the nurse take first?
Explanation
Choice A Reason: Observing for cerebrospinal fluid (CSF) leaks from the evacuation site is important, but not the first action that the nurse should take. CSF leaks can indicate a breach in the dura mater, which can increase the risk of infection and meningitis. The nurse should inspect the dressing and the nose and ears for any clear or bloody drainage, and report any findings to the provider. However, these measures are secondary to ensuring adequate oxygenation and perfusion.
Choice B Reason: Checking the oximeter is also important, but not the first action that the nurse should take. The oximeter measures the oxygen saturation of the blood, which reflects the adequacy of gas exchange in the lungs. The nurse should maintain the oxygen saturation above 90%, and administer supplemental oxygen as prescribed.
However, these measures are secondary to ensuring adequate oxygenation and perfusion.
Choice C Reason: Assessing for an increase in temperature is another important action, but not the first one that the nurse should take. An increase in temperature can indicate an infection, inflammation, or damage to the hypothalamus, which can affect the thermoregulation of the body. The nurse should monitor the temperature and administer antipyretics as prescribed. However, these measures are secondary to ensuring adequate oxygenation and perfusion.
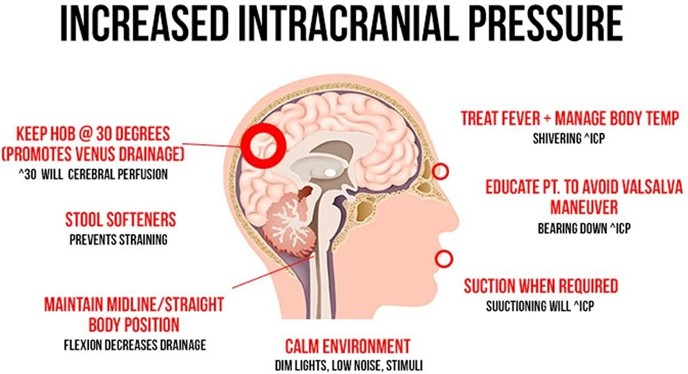
Choice D Reason: Monitoring for manifestations of increased intracranial pressure is the first action that the nurse should take. Increased intracranial pressure can result from bleeding, swelling, or fluid accumulation in the brain, which can compress and damage brain tissue and blood vessels. The nurse should assess for signs and symptoms of increased intracranial pressure, such as headache, nausea, vomiting, altered level of consciousness, pupillary changes, or Cushing's triad (bradycardia, hypertension, and irregular respirations). The nurse should also intervene to prevent or reduce increased intracranial pressure, such as elevating the head of the bed, maintaining normothermia, and administering osmotic diuretics. Monitoring for manifestations of increased intracranial pressure is essential to prevent further brain injury and preserve neurological function.
A nurse is monitoring a client who was admited with a severe burn injury and is receiving IV fluid resuscitation therapy. The nurse should identify a decrease in which of the following findings as an indication of adequate fluid replacement?
Explanation
Choice A Reason: Urine output is not a finding that should decrease with adequate fluid replacement. On the contrary, urine output should increase as the fluid therapy restores the renal perfusion and function. The nurse should monitor the urine output and ensure that it is at least 0.5 mL/kg/hr for adults and 1 mL/kg/hr for children.
Choice B Reason: Heart rate is a finding that should decrease with adequate fluid replacement. A high heart rate is a sign of hypovolemia, which occurs when the burn injury causes fluid loss from the intravascular space. The nurse should monitor the heart rate and expect it to decrease as the fluid therapy replenishes the blood volume and improves the cardiac output.
Choice C Reason: Weight is not a finding that should decrease with adequate fluid replacement. On the contrary, weight may increase as the fluid therapy restores the hydration status and corrects the fluid deficit. The nurse should monitor the weight and compare it with the pre-burn weight to evaluate the fluid balance.
Choice D Reason: Blood pressure is not a finding that should decrease with adequate fluid replacement. On the contrary, blood pressure may increase as the fluid therapy restores the vascular tone and improves the tissue perfusion. The nurse should monitor the blood pressure and expect it to increase as the fluid therapy compensates for the fluid loss.
A nurse is caring for a client who has a traumatic head injury and is exhibiting signs of increasing intracranial pressure. Which of the following medications should the nurse plan to administer?
Explanation
Choice A Reason: Dextran 70 is not a medication that the nurse should plan to administer for a client who has a traumatic head injury and is exhibiting signs of increasing intracranial pressure. Dextran 70 is a plasma expander that increases the blood volume and viscosity, which can worsen the intracranial pressure by increasing the cerebral blood flow and edema.
Choice B Reason: Hydroxyethyl starch is not a medication that the nurse should plan to administer for a client who has a traumatic head injury and is exhibiting signs of increasing intracranial pressure. Hydroxyethyl starch is another plasma expander that has similar effects as dextran 70, and can also increase the risk of coagulopathy and renal failure.
Choice C Reason: Albumin 25% is not a medication that the nurse should plan to administer for a client who has a traumatic head injury and is exhibiting signs of increasing intracranial pressure. Albumin 25% is a colloid solution that increases the oncotic pressure and draws fluid from the interstitial space into the intravascular space, which can also worsen the intracranial pressure by increasing the cerebral blood flow and edema.
Choice D Reason: Mannitol 25% is a medication that the nurse should plan to administer for a client who has a traumatic head injury and is exhibiting signs of increasing intracranial pressure. Mannitol 25% is an osmotic diuretic that reduces the intracranial pressure by creating an osmotic gradient and drawing fluid from the brain tissue into the blood vessels, which can then be excreted by the kidneys. The nurse should monitor the urine output, serum osmolality, and electrolytes when administering mannitol 25%.
A nurse is caring for a client who has a deep vein thrombosis and is prescribed heparin by continuous IV infusion at 1,200 units/hr. Available is heparin 25,000 units in 500 mL D5W. The nurse should set the IV pump to deliver how many mL/hr?
(Round the answer to the nearest tenth/whole number. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
- To find the concentration of heparin in the solution, divide the amount of heparin by the volume of D5W: 25,000 units / 500 mL = 50 units/mL
- To find the infusion rate, divide the prescribed dose by the concentration: 1,200 units/hr / 50 units/mL = 24 mL/hr
- Round the answer to the nearest tenth/whole number: 24 mL/hr
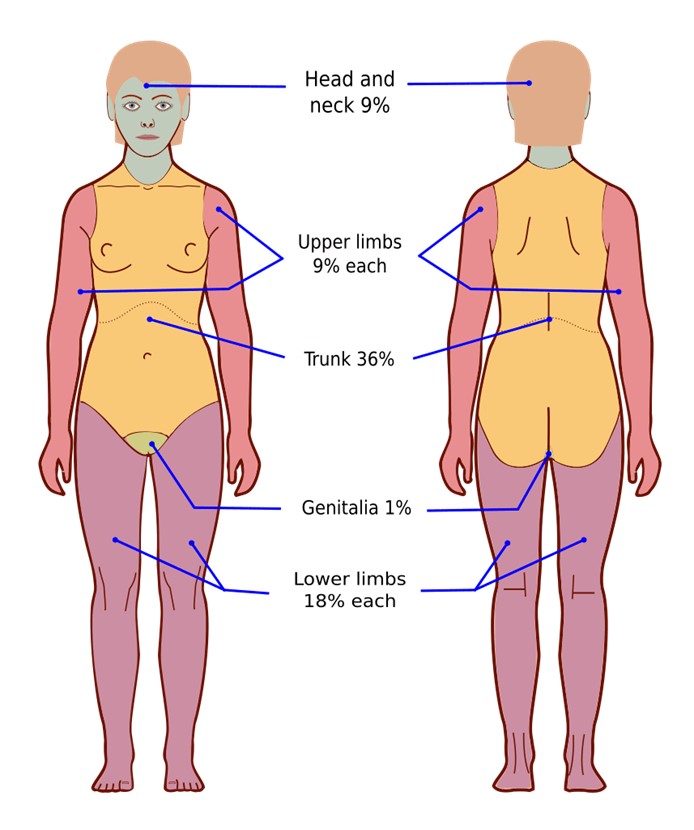
A nurse is assessing the depth and extent of injury on a client who has severe burns to the face, neck, and upper extremities. Which of the following factors is the nurse's priority when assessing the severity of the client's burns?
Explanation
Choice A Reason: Cause of the burn is not the nurse's priority when assessing the severity of the client's burns. The cause of the burn may indicate the type and duration of exposure, such as thermal, chemical, electrical, or radiation, which can affect the depth and extent of injury. However, these factors are secondary to ensuring adequate oxygenation and ventilation.
Choice B Reason: Age of the client is not the nurse's priority when assessing the severity of the client's burns. The age of the client may influence the response to burn injury, such as healing time, infection risk, and fluid requirements.
However, these factors are secondary to ensuring adequate oxygenation and ventilation.
Choice C Reason: Associated medical history is not the nurse's priority when assessing the severity of the client's burns. The associated medical history may affect the outcome and prognosis of burn injury, such as pre-existing conditions, medications, or allergies. However, these factors are secondary to ensuring adequate oxygenation and ventilation.
Choice D Reason: Location of the burn is the nurse's priority when assessing the severity of the client's burns. The location of the burn can indicate the potential for life-threatening complications, such as airway obstruction, inhalation injury, or impaired circulation. The nurse should assess for signs and symptoms of respiratory distress, such as stridor, wheezes, or cyanosis, and prepare for endotracheal intubation if needed. The nurse should also monitor for signs and symptoms of compartment syndrome, such as pain, pallor, paresthesia, pulselessness, or paralysis, and report any findings to the provider. The location of the burn can also affect the functional and cosmetic outcomes, such as vision loss, facial disfigurement, or joint contractures. The nurse should provide appropriate wound care, pain management, and rehabilitation as prescribed. Assessing for location of burn is essential to prevent further injury and preserve vital functions.
A nurse is caring for a client who is experiencing Cushing's triad following a subdural hematoma. Which of the following medications should the nurse plan to administer?
Explanation
Choice A Reason: Albumin 25% is not a medication that the nurse should plan to administer for a client who is experiencing Cushing's triad following a subdural hematoma. Albumin 25% is a colloid solution that increases the oncotic pressure and draws fluid from the interstitial space into the intravascular space, which can worsen the intracranial pressure by increasing the cerebral blood flow and edema.
Choice B Reason: Dextran 70 is not a medication that the nurse should plan to administer for a client who is experiencing Cushing's triad following a subdural hematoma. Dextran 70 is a plasma expander that increases the blood volume and viscosity, which can also worsen the intracranial pressure by increasing the cerebral blood flow and edema.
Choice C Reason: Mannitol 25% is a medication that the nurse should plan to administer for a client who is experiencing Cushing's triad following a subdural hematoma. Mannitol 25% is an osmotic diuretic that reduces the intracranial pressure by creating an osmotic gradient and drawing fluid from the brain tissue into the blood vessels, which can then be excreted by the kidneys. The nurse should monitor the urine output, serum osmolality, and electrolytes when administering mannitol 25%.
Choice D Reason: Hydroxyethyl starch is not a medication that the nurse should plan to administer for a client who is experiencing Cushing's triad following a subdural hematoma. Hydroxyethyl starch is another plasma expander that has similar effects as dextran 70, and can also increase the risk of coagulopathy and renal failure.
You just viewed 10 questions out of the 70 questions on the ATI Med Surg Custom N235 Final Summer 2023 Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



