A nurse in the emergency department is caring for a client who has extensive partial and full-thickness burns of the head, neck, and chest. While planning the client's care, the nurse should identify which of the following risks as the priority for assessment and intervention?
Infection
Airway obstruction
Paralytic ileus
Fluid imbalance
The Correct Answer is B
Choice A Reason: Infection is a serious complication of burn injuries, but not the priority risk for assessment and intervention. The nurse should monitor the client's wound healing, temperature, white blood cell count, and signs of sepsis, and administer antibiotics as prescribed. However, these measures are secondary to ensuring adequate oxygenation and ventilation.
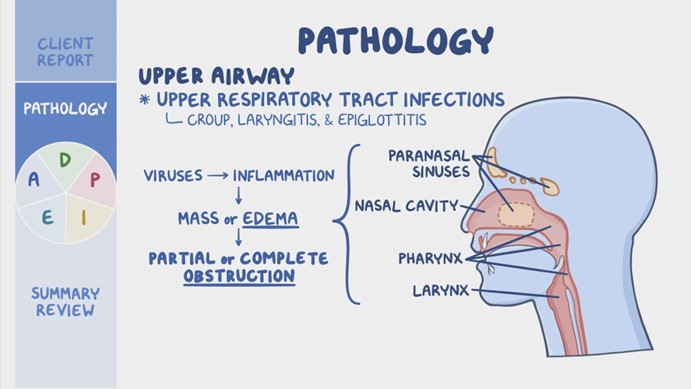
Choice B Reason: Airway obstruction is the priority risk for assessment and intervention for a client who has burns of the head, neck, and chest. The nurse should assess the client's airway patency, respiratory rate, oxygen saturation, breath sounds, and signs of respiratory distress, such as stridor, wheezes, or cyanosis. The nurse should also provide humidified oxygen, suction secretions, elevate the head of the bed, and prepare for endotracheal intubation if needed. Airway obstruction can occur due to edema, inflammation, or inhalation injury of the upper airway, and can quickly lead to hypoxia, respiratory failure, and death.
Choice C Reason: Paralytic ileus is a potential complication of burn injuries, but not the priority risk for assessment and intervention. The nurse should assess the client's bowel sounds, abdominal distension, nausea, vomiting, and stool output, and administer fluids, electrolytes, and nutritional support as prescribed. However, these measures are secondary to ensuring adequate oxygenation and ventilation.
Choice D Reason: Fluid imbalance is another potential complication of burn injuries, but not the priority risk for assessment and intervention. The nurse should assess the client's fluid status, urine output, vital signs, weight, and serum electrolytes, and administer intravenous fluids as prescribed. However, these measures are secondary to ensuring adequate oxygenation and ventilation.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A Reason: Dextran 70 is not a medication that the nurse should plan to administer for a client who has a traumatic head injury and is exhibiting signs of increasing intracranial pressure. Dextran 70 is a plasma expander that increases the blood volume and viscosity, which can worsen the intracranial pressure by increasing the cerebral blood flow and edema.
Choice B Reason: Hydroxyethyl starch is not a medication that the nurse should plan to administer for a client who has a traumatic head injury and is exhibiting signs of increasing intracranial pressure. Hydroxyethyl starch is another plasma expander that has similar effects as dextran 70, and can also increase the risk of coagulopathy and renal failure.
Choice C Reason: Albumin 25% is not a medication that the nurse should plan to administer for a client who has a traumatic head injury and is exhibiting signs of increasing intracranial pressure. Albumin 25% is a colloid solution that increases the oncotic pressure and draws fluid from the interstitial space into the intravascular space, which can also worsen the intracranial pressure by increasing the cerebral blood flow and edema.
Choice D Reason: Mannitol 25% is a medication that the nurse should plan to administer for a client who has a traumatic head injury and is exhibiting signs of increasing intracranial pressure. Mannitol 25% is an osmotic diuretic that reduces the intracranial pressure by creating an osmotic gradient and drawing fluid from the brain tissue into the blood vessels, which can then be excreted by the kidneys. The nurse should monitor the urine output, serum osmolality, and electrolytes when administering mannitol 25%.
Correct Answer is A
Explanation
Choice A Reason: This is correct because respiratory acidosis is characterized by a low pH and a high PaCO2, indicating that the client has impaired ventilation and excess carbon dioxide in the blood.
Choice B Reason: This is incorrect because respiratory alkalosis is characterized by a high pH and a low PaCO2, indicating that the client has increased ventilation and reduced carbon dioxide in the blood.
Choice C Reason: This is incorrect because metabolic acidosis is characterized by a low pH and a low HCO3, indicating that the client has an excess of metabolic acids or a loss of base in the blood.
Choice D Reason: This is incorrect because metabolic alkalosis is characterized by a high pH and a high HCO3, indicating that the client has an excess of base or a loss of metabolic acids in the blood.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
