RN Pharmacology 2023 IV
ATI RN Pharmacology 2023 IV
Total Questions : 67
Showing 10 questions Sign up for moreA nurse is caring for a client in an outpatient clinic.
Complete the following sentence by using the lists of options.
The client is at risk for
Explanation
The client is at risk for decreased absorption due to medication interactions.
Rationale
Esomeprazole works by reducing the production of stomach acid, thereby raising the pH level in the stomach. Levothyroxine, like many other medications, is absorbed primarily in the upper part of the small intestine where a more acidic environment is optimal for absorption. When stomach acid production is reduced by esomeprazole, the pH of the stomach increases, which can decrease the dissolution and absorption of levothyroxine.
A nurse is caring for a female client in a provider's office.
The nurse notifies the client and provides teaching about the newly prescribed medication. For each of the statements made by the client, click to specify whether the statement indicates an understanding or no understanding of the teaching provided.
Explanation
A. This statement indicates that the client understands that black stools can indicate gastrointestinal bleeding, a potential side effect of iron supplementation. Notifying the provider is appropriate in this case to assess for any significant bleeding.
B. Taking the medication with orange juice can increase iron absorption due to the vitamin C content.
D. Antacids can reduce the absorption of iron supplements. Therefore, avoiding taking antacids close to the time of taking iron supplements is recommended to ensure optimal absorption.
C. While some iron supplements are best absorbed on an empty stomach, Ferrous Sulfate is typically recommended to be taken with food to reduce gastrointestinal side effects. Taking it on an empty stomach might increase the risk of stomach upset.
E. This statement does not directly relate to iron supplementation. Iron supplements do not typically require rinsing the mouth afterward.
Explanation
A. Elevating the affected extremity can help reduce swelling and promote venous return. This action can aid in reducing the discomfort associated with phlebitis. However, this is not the first action.
B Slowing down the infusion rate can decrease the irritation to the vein caused by the IV fluids, which might contribute to the development or exacerbation of phlebitis. Slowing down the flow rate can help reduce this risk and allow the vein to recover. However, this is not the first action.
C. Applying a cool compress can help reduce inflammation and discomfort at the IV site. Cold therapy can constrict blood vessels, reduce swelling, and provide temporary relief from pain and inflammation associated with phlebitis. It should be applied intermittently and not for extended periods to avoid potential complications like tissue damage.
D. Aspirating fluid from the catheter is not a recommended action for managing phlebitis. It does not address the underlying cause of inflammation and can potentially introduce air into the bloodstream or cause further trauma to the vein.
Explanation
B. Endocarditis is an infection of the inner lining of the heart chambers and valves, usually caused by bacteria entering the bloodstream. Treatment typically involves antibiotics that can penetrate into heart tissues to eradicate the infection.
A. Kidney transplant recipients are at risk for infections, particularly from immunosuppressive therapy that reduces their ability to fight off pathogens. Metronidazole is not commonly indicated.
C. Metronidazole can rarely cause neurotoxic side effects, including seizures, particularly with high doses or prolonged use. It is not used to treat seizures, and its use should be carefully monitored in patients with a history of seizures or neurological disorders.
D. Hypokalemia is a metabolic disorder that requires correction of potassium levels through appropriate supplementation or treatment of the underlying cause. Metronidazole is used for infections and does not play a role in managing electrolyte abnormalities like hypokalemia.
A nurse in a provider's office is caring for a client.
What actions should the nurse take?
Select all that apply.
Explanation
C. Thiazide diuretics like hydrochlorothiazide can cause orthostatic hypotension, which may contribute to the client's symptoms of dizziness and light-headedness upon standing. Advising the client to change positions slowly can help mitigate these symptoms by allowing the body time to adjust to changes in posture and blood pressure.
D. Thiazide diuretics can alter electrolyte levels, including potassium, which is critical for normal cardiac function. Although the client's potassium level (3.4 mEq/L) is within the normal range, ongoing
monitoring for potential dysrhythmias is prudent due to the electrolyte-altering effects of hydrochlorothiazide.
E. Given the client's report of dizziness and light-headedness upon standing, checking for orthostatic hypotension is important. Thiazide diuretics can cause volume depletion and subsequent orthostatic hypotension, especially in older adults. Assessing blood pressure and symptoms in supine and standing positions will help evaluate for orthostatic changes.
A. This is not typically recommended for hydrochlorothiazide. It is usually advised to take this medication in the morning to avoid nighttime diuresis and nocturia. Therefore, this action is not appropriate.
B. Hydrochlorothiazide is a thiazide diuretic that can cause potassium loss through increased urine output. Restricting potassium intake is not typically necessary unless potassium levels drop significantly below the normal range. Given that the client's potassium level is within the normal range (3.4 mEq/L), advising strict potassium restriction is not indicated at this time.
Explanation
B. Immobility can significantly affect bone health and metabolism, leading to osteoporosis or exacerbating existing osteoporosis. Alendronate is generally indicated to treat osteoporosis by increasing bone density, but its effectiveness may be compromised if the patient is severely immobilized.
A. Paget's disease of bone is a condition where bone remodeling is abnormal, leading to weakened and deformed bones. Although alendronate is not typically contraindicated in patients with Paget's disease, caution may be warranted due to potential interactions or considerations about bone metabolism. This finding does not directly pose a safety risk specific to alendronate use unless there are other underlying factors related to bone health or metabolism that need consideration.
C. Anaphylaxis is a severe allergic reaction that typically involves multiple body systems and can be life- threatening. Alendronate itself does not typically cause allergic reactions like anaphylaxis.
D. Postmenopausal status is a common indication for alendronate use. After menopause, women are at increased risk of osteoporosis due to decreased estrogen levels, which accelerates bone loss.
Alendronate is specifically used to treat osteoporosis in postmenopausal women by slowing down bone breakdown and increasing bone mass.
A nurse is teaching a client who has a prescription for an epinephrine auto-injector. The nurse should instruct the client to take which of the following actions first?
Explanation
B. This action refers to the correct technique of using an epinephrine auto-injector. The device should be jabbed firmly into the outer thigh muscle. Jabbing the auto-injector into the thigh ensures that the needle is properly inserted into the muscle to deliver the epinephrine dose promptly. This action should be swift and decisive to ensure proper delivery of the medication.
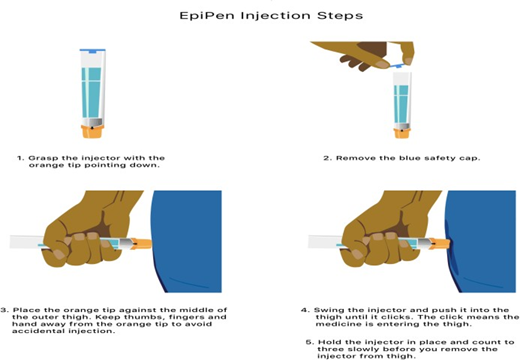
A. Massaging the thigh before administering epinephrine is not recommended and is not part of the proper technique for using an auto-injector.
C. While seeking medical attention is crucial after administering epinephrine, it is not the first action to take. Epinephrine should be administered immediately upon recognizing signs of anaphylaxis, as it rapidly reverses severe symptoms such as difficulty breathing and low blood pressure.
D. After injecting the epinephrine, the auto-injector should be held in place for a few seconds (typically 3 to 10 seconds) to ensure that the full dose of medication is delivered.
Explanation
A. Nitroglycerin is commonly used to treat angina (chest pain) and works by dilating blood vessels to increase blood flow to the heart. Both sildenafil and nitroglycerin can cause vasodilation, leading to a significant drop in blood pressure. Concomitant use of sildenafil with nitroglycerin or other nitrates is contraindicated due to the risk of severe hypotension (dangerously low blood pressure) and cardiovascular collapse.
B. Albuterol is a bronchodilator used to treat asthma and COPD by relaxing the airway muscles. It does not have significant interactions with sildenafil related to blood pressure.
C. Furosemide is a loop diuretic used to treat fluid retention (edema) and hypertension by increasing urine output. Furosemide does not have specific contraindications with sildenafil. While both
medications can cause a decrease in blood pressure, the concurrent use of furosemide and sildenafil is typically managed by monitoring for signs of hypotension rather than being contraindicated outright.
D. Indomethacin is a nonsteroidal anti-inflammatory drug (NSAID) used to treat pain and inflammation by inhibiting prostaglandin synthesis. Indomethacin does not have specific contraindications with sildenafil. While NSAIDs can potentially cause renal impairment and fluid retention, leading to increased blood pressure, this is not a direct contraindication for the use of sildenafil.
Explanation
A. Warming the PN formula to room temperature is a routine practice to make it more comfortable for administration but does not directly address hyperkalemia.
B. Lactose-free formulas may be requested for clients who have lactose intolerance or other specific dietary needs but are not directly related to hyperkalemia.
C. IV dextrose (usually in the form of dextrose 5% in water, D5W) can be used to temporarily shift potassium from the extracellular space into the cells, thereby lowering serum potassium levels. Dextrose helps in stimulating insulin release, which facilitates potassium uptake into cells, effectively lowering serum potassium levels. However, it is not the immediate action.
D. Hyperkalemia can lead to serious cardiac arrhythmias due to its effects on myocardial cell membrane potentials. Therefore, close cardiac monitoring is essential to detect any signs of cardiac instability.
A nurse is teaching a client who has a new prescription for a metered-dose inhaler. Which of the following instructions should the nurse include in the teaching? (Select all that apply.)
Explanation
A. Spacers are devices that can be attached to MDIs to help improve medication delivery to the lungs. They reduce the need for precise coordination between inhalation and actuation, making it easier for the medication to reach the lungs.
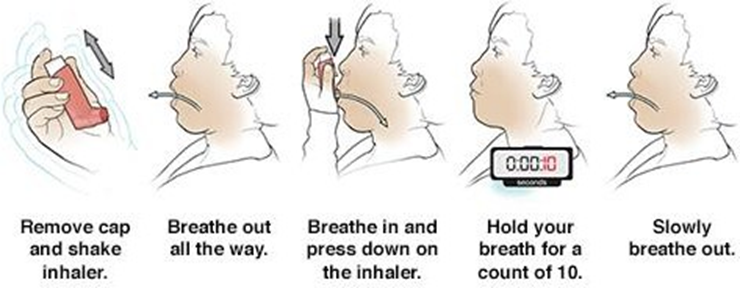
B Inhaling slowly allows the medication to be dispersed and distributed more effectively throughout the lungs. Rapid inhalation may cause the medication to impact the back of the throat rather than reaching the lungs. Instructing the client to inhale slowly helps maximize the amount of medication that reaches the airways.
C. Holding the mouthpiece between the lips and forming a good seal with the lips helps ensure that the medication is delivered directly into the airways. This technique ensures that the client inhales the medication effectively. Holding the mouthpiece between the lips also prevents the medication from escaping and ensures that it reaches the lungs.
E. Some medications delivered via MDIs, especially corticosteroids, can cause oral candidiasis (thrush) or irritation if not rinsed out of the mouth. Rinsing the mouth with water after using the MDI helps reduce the risk of side effects such as thrush or irritation in the mouth and throat. This instruction is particularly important for clients using corticosteroid inhalers.
D. MDIs can deliver medications for both quick relief (short-acting bronchodilators) and long-term control (maintenance medications). This instruction is correct if the medication prescribed is a short- acting bronchodilator (e.g., albuterol) used for quick relief of symptoms like wheezing or shortness of breath. However, if the medication is a long-term control medication (e.g., corticosteroid inhaler), it should be used regularly as prescribed to manage underlying inflammation.
You just viewed 10 questions out of the 67 questions on the ATI RN Pharmacology 2023 IV Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



