Nightdale College HESI Pharmacology RN
Nightdale College HESI Pharmacology RN
Total Questions : 47
Showing 10 questions Sign up for moreA client with psychosis who is receiving an antipsychotic medication is continually rubbing the back of the neck. Which nursing intervention is best for the nurse to implement?
Explanation
Choice A reason: Providing a heating pad to the client may provide some temporary relief, but it does not address the underlying cause of the neck discomfort, which is likely due to extrapyramidal side effects (EPS) of the antipsychotic medication.
Choice B reason: Obtaining a prescription for physical therapy services may be beneficial for the client's overall health and well-being, but it is not the best intervention for the acute problem of neck discomfort. Physical therapy may also require a referral and a waiting period, which would delay the relief for the client.
Choice C reason: Giving a PRN prescription for benztropine is the best intervention for the nurse to implement, as benztropine is an anticholinergic medication that can counteract the EPS of the antipsychotic medication. Benztropine can reduce the muscle stiffness and spasms that cause the neck discomfort.
Choice D reason: Obtaining an extra pillow for the client to use at night may help the client sleep better, but it does not address the neck discomfort during the day. It also does not treat the EPS of the antipsychotic medication, which may worsen over time.
Explanation
Choice A reason: Taking levothyroxine on an empty stomach ensures better absorption and prevents interference from food or other medications. The client should take levothyroxine at least 30 minutes before breakfast or four hours after the last meal of the day.
Choice B reason: Consuming foods that are high in iodine is not recommended for clients taking levothyroxine, as it may affect the thyroid function and the dosage of the medication. Foods that are high in iodine include seafood, seaweed, dairy products, and iodized salt.
Choice C reason: Administering levothyroxine at bedtime is not advisable, as it may cause insomnia, anxiety, or palpitations. Levothyroxine is best taken in the morning, as it mimics the natural secretion of thyroid hormones.
Choice D reason: Avoiding the use of iron supplements is not necessary for clients taking levothyroxine, as long as they are taken at different times. Iron supplements can interfere with the absorption of levothyroxine, so they should be taken at least four hours apart.
Explanation
Choice A reason: Baclofen is a muscle relaxant that can cause drowsiness, dizziness, and orthostatic hypotension. These side effects can increase the risk of falls and injuries for the client. Therefore, the nurse should advise the client to move slowly and cautiously when rising and walking, and to use assistive devices if needed.
Choice B reason: Evaluating muscle strength every 4 hours is not the most important intervention for the nurse to implement, as baclofen does not affect muscle strength directly. It may reduce muscle spasticity and stiffness, but it does not improve muscle function or coordination.
Choice C reason: Monitoring intake and output every 8 hours is not the most important intervention for the nurse to implement, as baclofen does not have a significant effect on fluid balance or renal function. However, the nurse should monitor the client for signs of urinary retention, which is a rare but possible adverse effect of baclofen.
Choice D reason: Ensuring the client knows to stop baclofen before using other antispasmodics is not the most important intervention for the nurse to implement, as baclofen can be used in combination with other antispasmodics under medical supervision. However, the nurse should educate the client about the potential drug interactions and contraindications of baclofen, and to consult the prescriber before taking any new medications.
Explanation
Choice A reason: Spinach and other green vegetables are rich in vitamin K, which is essential for blood clotting. However, dabigatran is not affected by vitamin K intake, unlike warfarin, another anticoagulant drug. Therefore, there is no need to eliminate these foods from the diet.
Choice B reason: Dabigatran does not require routine laboratory monitoring of bleeding parameters, such as prothrombin time (PT) or international normalized ratio (INR), unlike warfarin. Therefore, the client does not need to continue obtaining scheduled laboratory bleeding tests.
Choice C reason: Dabigatran is a direct thrombin inhibitor that prevents the formation of fibrin, the main component of blood clots. In case of a major bleeding event, the antidote for dabigatran is idarucizumab, a monoclonal antibody that binds to dabigatran and reverses its effect. However, this antidote is not readily available in most settings and should only be administered by a health care provider. Therefore, the client should not keep an antidote available at home.
Choice D reason: NSAIDs, such as ibuprofen or naproxen, can increase the risk of bleeding by inhibiting platelet aggregation and damaging the gastric mucosa. Therefore, the client should avoid using these drugs while taking dabigatran. The client should consult with the prescriber before taking any other medications, including over-the-counter or herbal products.
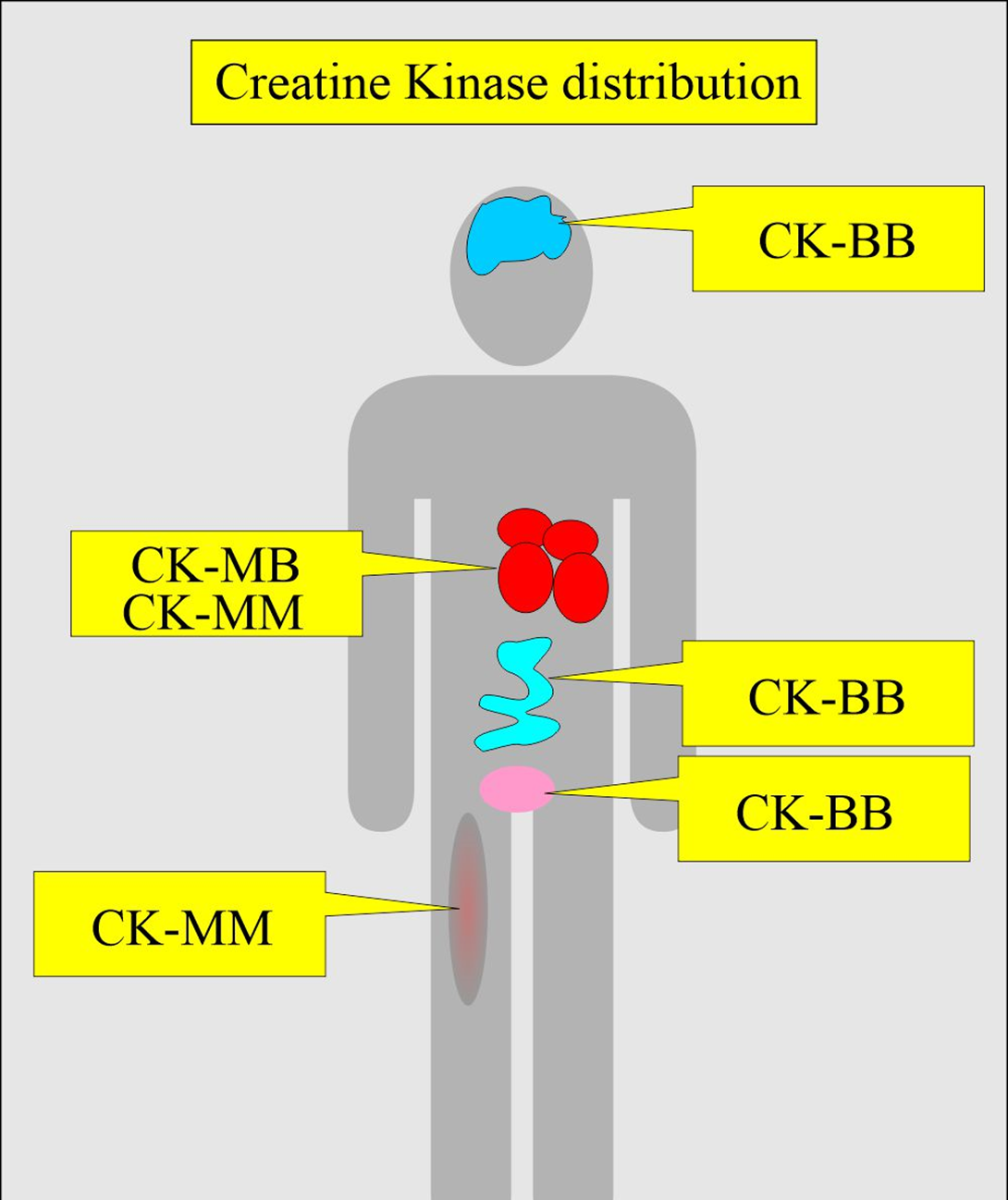
A client taking atorvastatin develops an increased serum creatine phosphokinase (CK) level. The nurse should assess the client for the onset of which problem?
Explanation
Choice A reason: Muscle tenderness is a sign of myopathy, a rare but serious adverse effect of atorvastatin and other statins. Myopathy is characterized by muscle weakness, pain, and elevated CK levels. CK is an enzyme that is released when muscle tissue is damaged. The nurse should monitor the client for muscle tenderness and report any changes to the prescriber.
Choice B reason: Nausea and vomiting are common side effects of atorvastatin, but they are not related to CK levels. The nurse should advise the client to take the medication with food and fluids to minimize gastrointestinal discomfort.
Choice C reason: Excessive bruising is not a typical side effect of atorvastatin, nor is it associated with CK levels. The nurse should assess the client for other possible causes of bleeding, such as coagulation disorders, trauma, or drug interactions.
Choice D reason: Peripheral edema is not a common side effect of atorvastatin, and it is not related to CK levels. The nurse should assess the client for other signs of fluid retention, such as weight gain, shortness of breath, or jugular venous distension. The nurse should also check the client's blood pressure and heart rate, as peripheral edema may indicate heart failure or hypertension.
The nurse is planning care for a client with major depression who is receiving a new prescription for duloxetine. Which information is most important for the nurse to obtain?
Explanation
The correct answer is b. Liver function laboratory results.
Choice A reason:
Weight change in the last month can be an important factor to consider for a patient's overall health and may be relevant in the context of depression, as significant weight changes can be a symptom of this condition. However, it is not the most critical piece of information before prescribing duloxetine. Duloxetine is not primarily metabolized by the kidneys, and while weight can affect dosing and efficacy, it is not the most crucial factor to consider before starting treatment.
Choice B reason:
Liver function laboratory results are crucial to obtain before prescribing duloxetine because duloxetine is extensively metabolized by the liver. The prescribing information for duloxetine warns of the potential for hepatotoxicity, and hepatic failure has been reported in some cases. Therefore, it is essential to ensure that the patient's liver function is normal before initiating therapy with duloxetine, as impaired liver function could lead to increased levels of the medication in the body and a higher risk of side effects.
Choice C reason:
Recent use of other antidepressants is important to consider avoiding drug interactions, particularly with monoamine oxidase inhibitors (MAOIs), which can lead to serious, life-threatening side effects if taken together with duloxetine. While this information is important, it is not as critical as liver function, because the primary concern with other antidepressants is the timing of medication changes rather than an absolute contraindication.
Choice D reason:
A family history of mental illness can provide valuable information for understanding a patient's background and potential genetic predispositions to certain conditions. However, this information does not directly impact the safety and initial prescribing of duloxetine. It may be more relevant for long-term treatment considerations and prognosis rather than immediate prescription safety.
Explanation
Choice A reason: Measuring the client's urinary output is not the most appropriate action for the nurse to take. Although urinary output is an important indicator of renal function, it is not related to the color change of the urine. The nurse should monitor the client's fluid balance as part of the routine care, but it is not a priority.
Choice B reason: Explaining the color change is normal is the most appropriate action for the nurse to take. Carbidopa/levodopa can cause the urine to become dark brown or black, which is a harmless side effect. The nurse should reassure the client that this is not a sign of a serious problem and does not affect the effectiveness of the medication.
Choice C reason: Obtaining a specimen for a urine culture is not the most appropriate action for the nurse to take. A urine culture is used to diagnose a urinary tract infection (UTI), which is characterized by symptoms such as dysuria, frequency, urgency, and hematuria. The color change of the urine due to carbidopa/levodopa is not indicative of a UTI. The nurse should obtain a urine culture only if the client has signs or symptoms of a UTI.
Choice D reason: Encouraging an increase in oral intake is not the most appropriate action for the nurse to take. Although adequate hydration is important for the client's health, it is not related to the color change of the urine. The nurse should encourage the client to drink enough fluids to prevent dehydration, but it is not a priority.
Explanation
Choice A reason: Employed as a construction worker is not the most important assessment finding for the nurse to address. Although the client's occupation may expose them to moist and warm environments that can promote fungal growth, it is not directly related to the administration of terbinafine HCL. The nurse should advise the client to wear breathable shoes and socks and keep the feet dry and clean, but it is not a priority.
Choice B reason: Reported history of alcoholism is the most important assessment finding for the nurse to address. Terbinafine HCL can cause hepatotoxicity, especially in clients with pre-existing liver disease or who consume alcohol regularly. The nurse should assess the client's liver function tests and alcohol intake before starting the medication and inform the prescriber accordingly. The nurse should also monitor the client for signs and symptoms of liver damage, such as jaundice, abdominal pain, nausea, or fatigue.
Choice C reason: White blood cell count of 8,500/mm3 (8.5 x 10^9/L) is not the most important assessment finding for the nurse to address. This value is within the normal reference range of 5,000 to 10,000/mm3 (5 to 10 x 10^9/L) and does not indicate any infection or inflammation. The nurse should check the client's baseline blood counts before starting the medication, but it is not a priority.
Choice D reason: Toenails appear thick and yellow is not the most important assessment finding for the nurse to address. This is a typical manifestation of a fungal toenail infection, which is the indication for terbinafine HCL. The nurse should expect the toenails to improve in appearance and texture after the completion of the treatment, which may take several weeks or months. The nurse should educate the client about the expected outcomes and adherence to the medication regimen, but it is not a priority.
Explanation
Choice A reason: Notifying the healthcare provider of the carbamazepine level is the most appropriate action for the nurse to take. Carbamazepine is an anticonvulsant drug that requires close monitoring of its serum levels to ensure therapeutic and safe effects. The normal reference range for carbamazepine is 4 to 12 mcg/mL or 16.9 to 50.8 mmol/L. A level of 84 mcg/L (35.6 mmol/L) is significantly higher than the upper limit and indicates toxicity. The nurse should report this finding to the prescriber immediately and hold the dose until further instructions.
Choice B reason: Administering the carbamazepine as prescribed is not the most appropriate action for the nurse to take. Giving the evening dose of carbamazepine when the morning level is already toxic can worsen the client's condition and cause serious adverse effects, such as confusion, drowsiness, ataxia, nystagmus, or coma. The nurse should not administer the medication without consulting the prescriber.
Choice C reason: Assessing the client for side effects of carbamazepine is an important action for the nurse to take, but it is not the most appropriate one. The nurse should assess the client for signs and symptoms of carbamazepine toxicity, such as nausea, vomiting, headache, blurred vision, or seizures. However, this action alone is not sufficient to address the problem. The nurse should also notify the prescriber and withhold the dose.
Choice D reason: Withholding this dose of the carbamazepine is a necessary action for the nurse to take, but it is not the most appropriate one. The nurse should not give the evening dose of carbamazepine when the morning level is already toxic, as this can increase the risk of complications. However, this action alone is not enough to resolve the issue. The nurse should also notify the prescriber and follow the appropriate interventions.
The health care provider prescribes the antibiotic tetracycline HCl for an adult client who arrived at an outpatient clinic. Which instruction should the nurse include in the teaching plan for this client?
Explanation
Choice A reason: Tetracycline HCl can cause photosensitivity, which increases the risk of sunburn and skin damage. The client should avoid direct sunlight and use sunscreen and protective clothing while taking the drug.
Choice B reason: Orange juice is acidic and can decrease the absorption of tetracycline HCl. The client should take the drug with water and avoid acidic foods and beverages.
Choice C reason: Serum drug levels are not routinely monitored for tetracycline HCl. The client should follow the prescribed dosage and duration of the therapy.
Choice D reason: Milk and antacids can interfere with the absorption of tetracycline HCl. The client should take the drug at least 1 hour before or 2 hours after meals and avoid dairy products and antacids.
You just viewed 10 questions out of the 47 questions on the Nightdale College HESI Pharmacology RN Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



