A client has undergone a surgical procedure and develops a weak, rapid pulse.
Which intervention should the nurse recommend to provider during their SBAR communication?
Anticholinergic.
Urinary catheter placement.
Beta blocker.
Intravenous fluid bolus.
The Correct Answer is D
A weak, rapid pulse indicates that the client is experiencing hypovolemia or low blood volume due to blood loss during surgery.
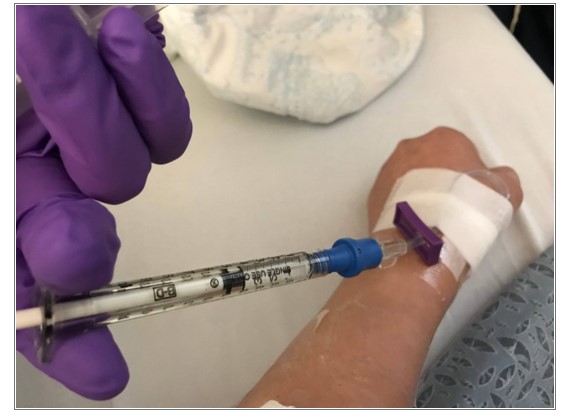
The nurse should recommend to the provider to administer intravenous fluids to restore the client’s circulating volume and improve their hemodynamic status.
Choice A is wrong because anticholinergics are drugs that block the action of acetylcholine, a neurotransmitter that stimulates the parasympathetic nervous system.
Anticholinergics can cause tachycardia, dry mouth, urinary retention, and blurred vision. They are not indicated for hypovolemia.
Choice B is wrong because urinary catheter placement is not a priority intervention for a client with hypovolemia.
Urinary catheterization can help monitor urine output and renal perfusion but does not address the underlying cause of low blood volume.
Choice C is wrong because beta blockers are drugs that block the action of epinephrine and norepinephrine, neurotransmitters that stimulate the sympathetic nervous system.
Beta-blockers can lower blood pressure, heart rate, and cardiac output.
They are not indicated for hypovolemia and can worsen the client’s condition.
To communicate this information using the SBAR tool, the nurse should follow these steps: Situation: Identify yourself, the client, and the problem.
For example: “I am (name), the nurse caring for (client name) in room (number).
I am calling because I am concerned that the client has developed hypovolemia after surgery.”
Background: Provide relevant and brief information related to the situation.
For example: “The client had a surgical procedure (name and type) at (time) today. They have lost (amount) of blood during and after surgery.
Their current vital signs are: blood pressure (value), pulse (value), respiratory rate (value), temperature (value), oxygen saturation (value).”
Assessment: Share your analysis and considerations of options. For
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
This outcome indicates that the client has resolved their constipation and has a regular pattern of defecation without difficulty or discomfort.
Choice A is wrong because taking a laxative daily can worsen constipation by causing dependency and reducing the natural peristalsis of the colon.
Choice C is wrong because requesting a bedpan every four hours does not necessarily mean that the client has bowel movements. It may indicate that the client has difficulty passing stool or has a sensation of incomplete emptying.
Choice D is wrong because having a bowel movement within 72 hours is still considered constipation. Constipation is diagnosed when bowel movements are associated with at least two of the following symptoms, occurring in the past three months with an onset of symptoms of at least six months: Less than three spontaneous bowel movements per week, Lumpy or hard stools from at least 25% of bowel movements.
Correct Answer is D
Explanation
30 to 40 mL/hour. This is the normal range of urine output for a typical adult client. The urine output should be at least 0.5 mL/kg/hour for adults.
Assuming an average weight of 70 kg, this would be 35 mL/hour.
Choice A is wrong because 5 to 10 mL/hour is too low and indicates oliguria, which is a sign of inadequate kidney function or dehydration.
Choice B is wrong because 12 to 15 mL/hour is also below the normal range and may indicate oliguria.
Choice C is wrong because 16 to 25 mL/hour is slightly below the normal range and may indicate reduced kidney perfusion or fluid intake.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
