A client reports having heartburn, dysphagia, and frequent dyspepsia. What does the nurse suspect that these clinical manifestations indicate?
Gastritis
GERD
Peptic ulcer disease
Pancreatitis
The Correct Answer is B
Choice A reason: Gastritis is not the most likely condition that these clinical manifestations indicate. Gastritis is an inflammation of the stomach lining, which can cause abdominal pain, nausea, vomiting, and loss of appetite. Gastritis may cause heartburn or dyspepsia, but it does not usually cause dysphagia, which is difficulty swallowing.
Choice B reason: GERD is the most likely condition that these clinical manifestations indicate. GERD stands for gastroesophageal reflux disease, which is a chronic condition where the stomach acid flows back into the esophagus, causing irritation and inflammation. GERD can cause heartburn, which is a burning sensation in the chest or throat, dysphagia, which is difficulty swallowing or a feeling of a lump in the throat, and dyspepsia, which is indigestion or discomfort in the upper abdomen.
Choice C reason: Peptic ulcer disease is not the most likely condition that these clinical manifestations indicate. Peptic ulcer disease is a condition where there are open sores or ulcers in the lining of the stomach or duodenum, which can cause bleeding, perforation, or obstruction. Peptic ulcer disease can cause dyspepsia, which is indigestion or discomfort in the upper abdomen, but it does not usually cause heartburn or dysphagia, which are more characteristic of GERD.
Choice D reason: Pancreatitis is not the most likely condition that these clinical manifestations indicate. Pancreatitis is an inflammation of the pancreas, which can cause severe abdominal pain, nausea, vomiting, fever, and jaundice. Pancreatitis does not cause heartburn, dysphagia, or dyspepsia, which are more characteristic of GERD.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
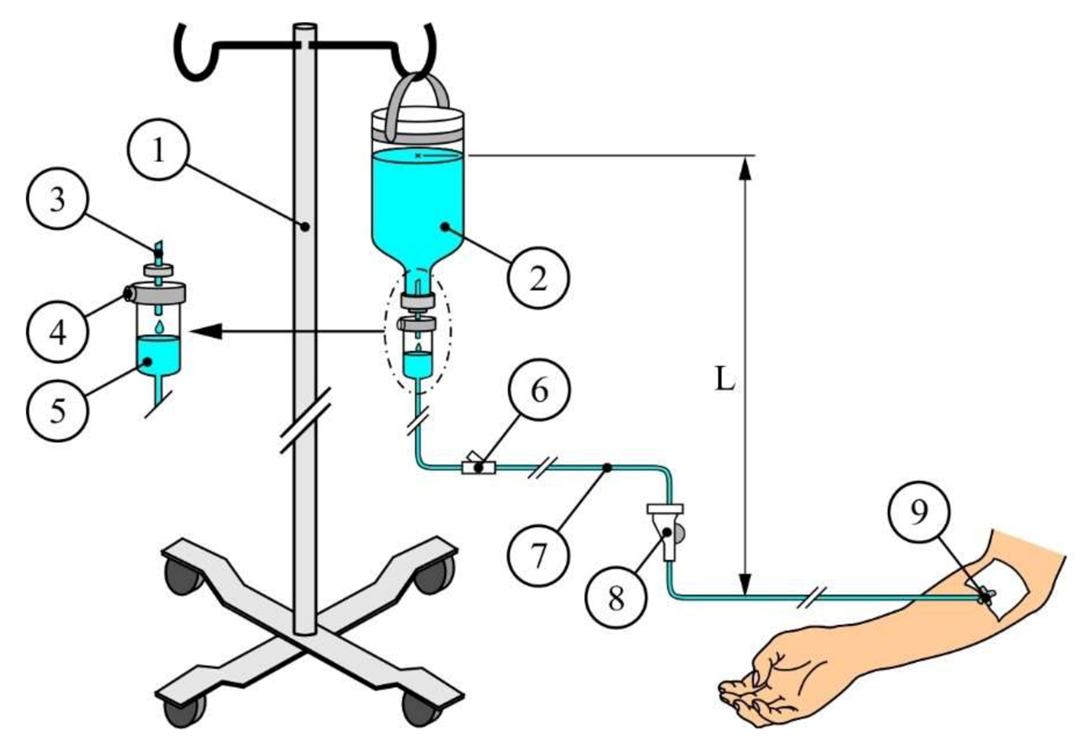
Choice A reason: This is a correct answer because normal saline is an isotonic solution, which means it has the same osmolarity as the blood plasma. It does not cause any fluid shifts between the intracellular and extracellular compartments, and it can help restore the fluid balance and the blood pressure of the dehydrated client.
Choice B reason: This is not a correct answer because 1/2 normal saline is a hypotonic solution, which means it has a lower osmolarity than the blood plasma. It causes fluid to shift from the extracellular to the intracellular compartment, which can lead to cellular swelling and edema. It is not suitable for rapid infusion, as it can cause hemolysis and hypotension.
Choice C reason: This is not a correct answer because D5W (5% Dextrose in Water) is an isotonic solution when it is in the IV bag, but it becomes hypotonic once it enters the body, as the dextrose is rapidly metabolized and only water remains. It causes fluid to shift from the extracellular to the intracellular compartment, which can lead to cellular swelling and edema. It is not suitable for rapid infusion, as it can cause hemolysis and hypotension.
Choice D reason: This is not a correct answer because D5 1/2 normal saline is a hypertonic solution, which means it has a higher osmolarity than the blood plasma. It causes fluid to shift from the intracellular to the extracellular compartment, which can lead to cellular shrinkage and dehydration. It is not suitable for rapid infusion, as it can cause hypernatremia and fluid overload.
Correct Answer is D
Explanation
Choice A reason: Excessive stomach acid secretion is not the correct answer because it is not a diagnostic test, but a possible cause of peptic ulcer disease. Peptic ulcers are sores that develop in the lining of the stomach or duodenum due to damage from stomach acid and digestive enzymes.
Choice B reason: An incompetent pyloric sphincter is not the correct answer because it is not a diagnostic test, but a possible complication of peptic ulcer disease. The pyloric sphincter is a muscular valve that controls the passage of food from the stomach to the small intestine. If it becomes damaged or weakened, it can cause gastric outlet obstruction, which is a blockage of the stomach.
Choice C reason: A metabolic acid-base imbalance is not the correct answer because it is not a diagnostic test, but a possible consequence of peptic ulcer disease. Peptic ulcers can cause bleeding, perforation, or gastric outlet obstruction, which can affect the acid-base balance of the body. For example, vomiting can cause metabolic alkalosis, which is a condition where the blood is too alkaline.
Choice D reason: An infection with Helicobacter pylori is the correct answer. Helicobacter pylori is a type of bacteria that can infect the stomach and duodenum and cause inflammation and ulcers. It is the most common cause of peptic ulcer disease. The health care provider can order a diagnostic test to detect the presence of Helicobacter pylori in the client's stomach or blood, such as a urea breath test, a stool antigen test, or a blood antibody test.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
