A client who is paraplegic is admitted with a foul smelling drainage from a sacral ulcer. The client is suspected to have a methicillin resistant Staphylococcus aureus (MRSA) infection. Which nursing intervention(s) should the nurse include in the plan of care? Select all that apply.
Use standard precautions and wear a mask.
Institute contact precautions for staff and visitors.
Send wound drainage for culture and sensitivity.
Explain the purpose of a low bacteria diet.
Monitor the client's white blood cell count.
Correct Answer : B,C,E
A. Use standard precautions and wear a mask.
While standard precautions should always be followed to prevent the spread of infection, wearing a mask is not specifically indicated for MRSA unless there is a risk of respiratory transmission. Contact precautions are more appropriate for MRSA.
B. Institute contact precautions for staff and visitors.
Contact precautions are necessary to prevent the spread of MRSA, a highly contagious bacteria. This involves using gloves and gowns when entering the client's room to prevent transmission of the bacteria to others.
C. Send wound drainage for culture and sensitivity.
Culturing the wound drainage helps identify the specific bacteria causing the infection and determines the most effective antibiotics for treatment (sensitivity testing).
D. Explain the purpose of a low bacteria diet.
A low bacteria diet is not typically indicated for managing MRSA infections. Instead, the focus should be on wound care, antibiotic therapy, and infection control measures to address the MRSA infection.
E. Monitor the client's white blood cell count.
Monitoring the white blood cell count helps assess the client's immune response and the severity of the infection. Elevated white blood cell counts may indicate an active infection and the need for further intervention.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["1"]
Explanation
To determine how many tablespoons the client should take with each dose, we need to first calculate the dosage in tablespoons based on the concentration of the oral suspension.
Given:
Dextromethorphan oral suspension concentration: 30 mg per 15 mL
To find out how many milliliters the client should take per dose:
The prescribed dose is 30 mg.
So, if 15 mL contains 30 mg, then 1 mL contains:
30 mg / 15 mL = 2 mg/mL
To find out how many milliliters the client should take for the prescribed dose:
30 mg / 2 mg/mL = 15 mL
Now, we know that the prescribed dose is 15 mL. To convert this to tablespoons, we can use the fact that 1 tablespoon (tbsp) is equal to 15 milliliters.
So, the client should take:
15 mL / 15 mL/tbsp = 1 tablespoon
Therefore, the nurse should instruct the client to take 1 tablespoon with each dose.
Correct Answer is A
Explanation
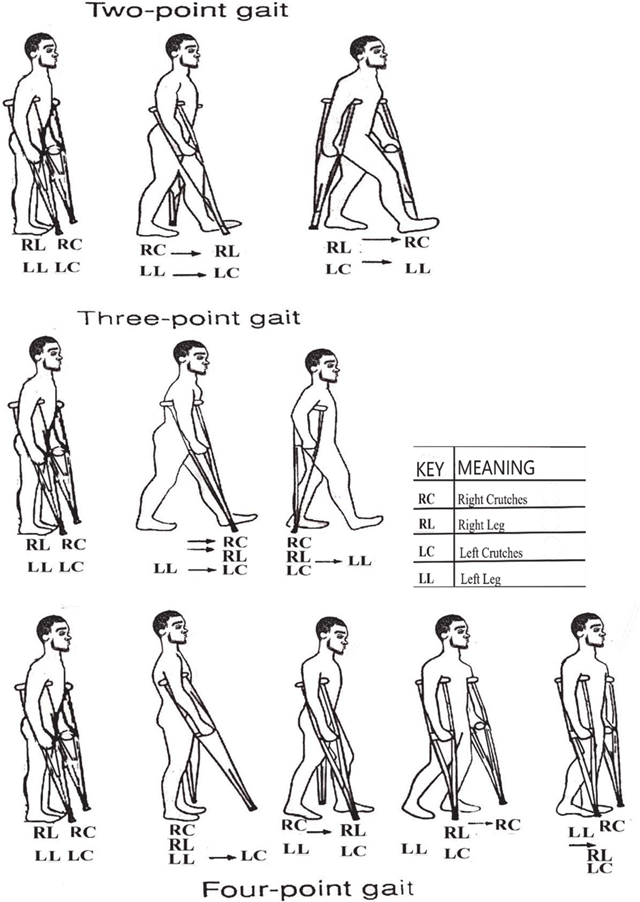
A. Progresses to foot touchdown and weight bearing of affected leg:
This choice indicates that the client understands proper crutch walking because it involves the correct progression of weight-bearing on the affected leg while using the crutches for support. In the three-point gait crutch walking technique, the client progresses by first touching down the foot of the affected leg and then transferring weight onto that leg while stepping forward with the crutches. This behavior ensures proper balance and support during ambulation.
B. Practices bicep and triceps isometric exercises:
This choice does not directly indicate understanding of proper crutch walking. While strengthening the biceps and triceps muscles can be beneficial for overall strength and endurance, it is not a specific behavior related to proper crutch walking technique.
C. Inspects crutches to ensure rubber tips are intact:
While it is important to inspect crutches regularly to ensure they are in good condition, this behavior alone does not necessarily indicate an understanding of proper crutch walking technique. It is more related to equipment maintenance and safety rather than the actual execution of crutch walking.
D. Bears body weight on the palms of hands during the crutch gait:
This choice suggests an incorrect technique. Proper crutch walking technique involves bearing weight on the hands through the hand grips of the crutches rather than the palms. Placing excessive weight on the palms can lead to discomfort, injury, and improper weight distribution, which could hinder effective ambulation.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
