A NICU nurse is completing an assessment on a premature infant male born at 29 weeks gestation. It is noted that the male infant has no palpable testes in the scrotum. The nurse should:
Document this expected finding.
Insert a urinary catheter to collect a urine specimen.
Initiate a social work consult.
Call the provider for this unexpected finding.
The Correct Answer is A
Choice A reason:
In premature infants, it is common for the testes to not be palpable in the scrotum at birth. This condition, known as cryptorchidism, affects about 30% of preterm infants1. The testes usually descend into the scrotum by the time the infant reaches term or within the first few months of life. Therefore, the nurse should document this as an expected finding and continue to monitor the infant’s development.
Choice B reason:
Inserting a urinary catheter to collect a urine specimen is not necessary in this situation. The absence of palpable testes in a premature infant is a common finding and does not indicate a need for immediate urinary evaluation. Urinary catheterization should be reserved for specific medical indications, such as suspected urinary tract infection or urinary retention.
Choice C reason:
Initiating a social work consult is not relevant to the clinical finding of undescended testes in a premature infant. Social work consultations are typically initiated for psychosocial issues, family support, or discharge planning. The absence of palpable testes is a medical finding that should be documented and monitored by the healthcare team.
Choice D reason:
Calling the provider for this unexpected finding is not necessary because the absence of palpable testes in a premature infant is an expected finding. The nurse should document the finding and continue to monitor the infant’s development. If the testes do not descend by the time the infant reaches term or within the first few months of life, further evaluation and management may be needed.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A reason:
Monitor your child’s temperature daily: Monitoring temperature is important for children with sickle cell anemia as they are prone to infections. A fever can be an early sign of infection, which can be serious for these children. Normal body temperature for children ranges from 36.5°C to 38°C. However, while monitoring temperature is important, it is not the most critical daily advice compared to ensuring adequate hydration.
Choice B Reason:
Restrict outdoor play to 1 hour per day: Limiting outdoor play is not typically necessary unless the child is experiencing extreme fatigue or pain. Physical activity is generally encouraged to maintain overall health, but it should be balanced with rest and hydration. Therefore, this advice is not as crucial as ensuring the child stays hydrated.
Choice C Reason:
Apply cold compresses when your child expresses pain: Cold compresses are not recommended for managing pain in sickle cell anemia. Instead, warm compresses or heating pads are often suggested to help relieve pain by improving blood flow. Cold can cause vasoconstriction, which may worsen pain and complications.
Choice D Reason:
Offer your child fluids frequently to meet their daily fluid goals: Staying well-hydrated is essential for children with sickle cell anemia. Adequate hydration helps prevent sickle cell crises by reducing blood viscosity and promoting better blood flow. This is the most appropriate and critical advice for daily care.
Correct Answer is ["A","C"]
Explanation
The correct answer is a. Vomiting, c. Tachycardia.
Choice A: Vomiting
Vomiting is a common symptom of thyroid storm. Thyroid storm is a life-threatening condition that occurs when the thyroid gland releases a large amount of thyroid hormone in a short period. This sudden surge in thyroid hormone can cause severe metabolic disturbances, leading to symptoms such as vomiting. Vomiting can result from the body’s attempt to cope with the excessive thyroid hormone levels, which can affect the gastrointestinal system.
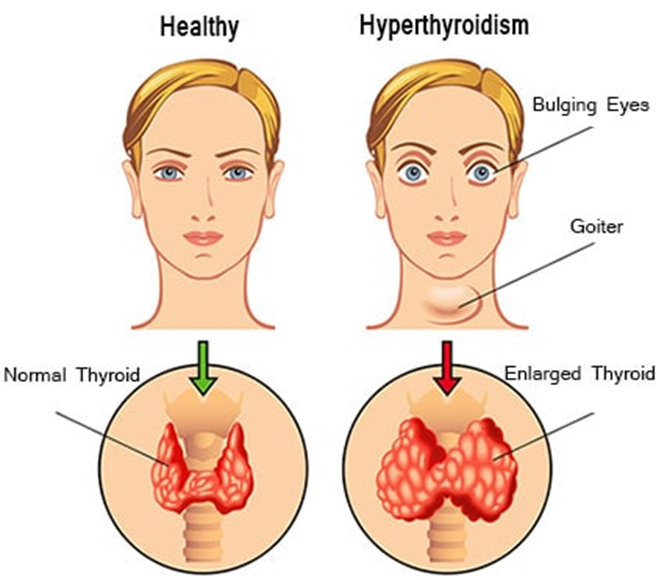
Choice B: Constipation
Constipation is not typically associated with thyroid storm. In fact, hyperthyroidism, including thyroid storm, usually causes an increase in bowel movements or diarrhea due to the accelerated metabolism. Constipation is more commonly associated with hypothyroidism, where the thyroid gland is underactive and slows down bodily functions.
Choice C: Tachycardia
Tachycardia, or a rapid heart rate, is a hallmark symptom of thyroid storm. The excessive thyroid hormones increase the body’s metabolic rate, leading to an increased demand for oxygen and nutrients. To meet this demand, the heart rate increases significantly, often exceeding 140 beats per minute. This rapid heart rate can be dangerous and requires immediate medical attention.
Choice D: Hypotension
Hypotension, or low blood pressure, is not a typical symptom of thyroid storm. Instead, thyroid storm often causes hypertension (high blood pressure) due to the increased metabolic activity and the body’s heightened demand for oxygen and nutrients. The cardiovascular system responds by increasing blood pressure to ensure adequate blood flow to vital organs.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
