A nurse is giving a change-of-shift report using SBAR to the oncoming nurse on a client who has a traumatic brain injury. Which of the following information should the nurse include in the background segment of SBAR?
Plan of care changes for the upcoming shift
Intracranial pressure readings
Glasgow results
Code status
The Correct Answer is D
Choice A reason: Plan of care changes for the upcoming shift
Plan of care changes for the upcoming shift are typically included in the “Recommendation” segment of SBAR. This section focuses on what actions need to be taken next, including any changes in the care plan that the oncoming nurse should be aware of. It ensures that the incoming nurse knows what to expect and what specific tasks or interventions are required during their shift.
Choice B reason: Intracranial pressure readings
Intracranial pressure (ICP) readings are crucial for monitoring a client with a traumatic brain injury. However, these readings are more appropriately included in the “Assessment” segment of SBAR. The assessment section provides an analysis of the client’s current condition, including vital signs, lab results, and other critical data. This information helps the oncoming nurse understand the client’s current status and any immediate concerns.
Choice C reason: Glasgow results
The Glasgow Coma Scale (GCS) results are used to assess the level of consciousness in clients with brain injuries. These results should also be included in the “Assessment” segment of SBAR. The GCS score provides valuable information about the client’s neurological status and helps guide clinical decisions. Including this information in the assessment ensures that the oncoming nurse has a clear understanding of the client’s current condition.
Choice D reason: Code status
Code status is a critical piece of information that should be included in the “Background” segment of SBAR. The background section provides relevant clinical history and context for the current situation. Knowing the client’s code status (e.g., full code, do not resuscitate) is essential for making informed decisions about their care, especially in emergency situations. Including this information in the background ensures that the oncoming nurse is aware of the client’s preferences and legal directives.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A reason: Induce Sedation
Pancuronium is not used to induce sedation. It is a neuromuscular blocking agent (NMBA) that causes paralysis of skeletal muscles. Sedation is typically achieved using medications such as benzodiazepines or propofol, which act on the central nervous system to produce a calming effect.
Choice B reason: Suppress Respiratory Effort
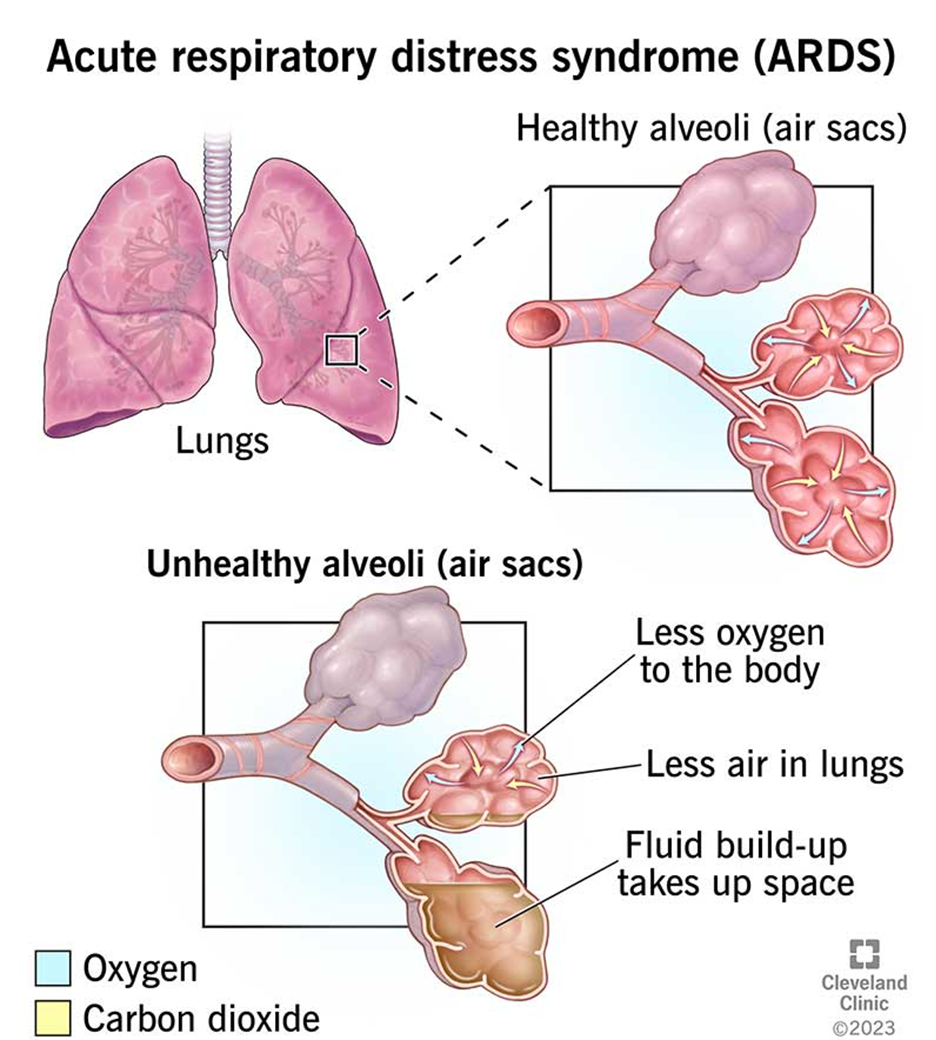
Pancuronium is used to suppress respiratory effort in patients with ARDS who require mechanical ventilation. By causing muscle paralysis, pancuronium helps to synchronize the patient’s breathing with the ventilator, reducing the risk of ventilator-induced lung injury and improving oxygenation. This is particularly important in severe cases of ARDS where patient-ventilator dyssynchrony can be detrimental.
Choice C reason: Decrease Chest Wall Compliance
Decreasing chest wall compliance is not a purpose of pancuronium. In fact, pancuronium does not directly affect chest wall compliance. Instead, it works by blocking the transmission of nerve impulses to the muscles, leading to muscle relaxation and paralysis.
Choice D reason: Decrease Respiratory Secretions
Pancuronium does not decrease respiratory secretions. Medications such as anticholinergics (e.g., atropine) are used to reduce secretions. Pancuronium’s primary role is to facilitate mechanical ventilation by ensuring complete muscle relaxation.
Correct Answer is ["A","E"]
Explanation
Choice A Reason: Administer acetaminophen
Administering acetaminophen is a common intervention for reducing fever. In this case, the child’s temperature has risen significantly from 37.3°C (99.1°F) at 0900 to 39.9°C (103.8°F) at 1300. A fever of 39.9°C is considered high and can cause discomfort and other complications if not managed. Acetaminophen is an antipyretic medication that helps lower body temperature and provides relief from fever. It is important to monitor the child’s temperature and ensure it returns to a normal range, which is typically around 36.5°C to 37.5°C (97.7°F to 99.5°F) for school-age children.
Choice B Reason: Have the child wear a mask
Having the child wear a mask is a preventive measure to reduce the spread of respiratory infections. While this intervention is important in certain contexts, such as during flu season or in the presence of contagious illnesses, it is not directly related to managing an acute asthma exacerbation. Masks can help prevent the spread of infections, but they do not address the immediate respiratory distress and wheezing observed in the child. Therefore, this choice is not the most appropriate intervention for the current situation.
Choice C Reason: Administer a dose of montelukast
Montelukast is a leukotriene receptor antagonist used for long-term management of asthma and allergic rhinitis. It helps reduce inflammation and prevent asthma attacks. However, montelukast is not typically used for immediate relief during an acute asthma exacerbation. It is more effective as a maintenance medication taken regularly to control chronic asthma symptoms. In this scenario, the child requires immediate relief from respiratory distress, making montelukast an inappropriate choice for acute intervention.
Choice D Reason: Encourage oral fluids
Encouraging oral fluids is a supportive measure to ensure the child remains hydrated. Hydration is important for overall health and can help thin mucus secretions, making it easier for the child to breathe. However, while hydration is beneficial, it is not the primary intervention needed to address the acute respiratory distress and wheezing observed in the child. Therefore, this choice alone is not sufficient to manage the current asthma exacerbation.
Respiratory system
Choice A Reason: Administer albuterol nebulizer
Administering an albuterol nebulizer is the most appropriate intervention for managing an acute asthma exacerbation. Albuterol is a short-acting beta-agonist that works by relaxing the muscles around the airways, allowing them to open up and improve airflow. This medication provides quick relief from symptoms such as wheezing, shortness of breath, and chest tightness. In this case, the child is experiencing respiratory distress and wheezing, making albuterol the most effective choice for immediate relief. The normal respiratory rate for school-age children is 18-25 breaths per minute, and the child’s rate of 26 breaths per minute indicates respiratory distress.
Choice B Reason: Evaluate the child’s peak flow
Evaluating the child’s peak flow involves measuring the maximum speed at which the child can exhale. This assessment helps determine the severity of the asthma exacerbation and the effectiveness of the treatment. Peak flow measurements can guide clinical decisions and adjustments to the child’s asthma management plan. However, during an acute asthma attack, the priority is to provide immediate relief from symptoms. While peak flow evaluation is valuable for ongoing asthma management, it is not the primary intervention needed to address the acute respiratory distress and wheezing observed in the child.
Choice C Reason: Initiate chest percussions
Initiating chest percussions involves rhythmic tapping on the chest to help loosen and mobilize mucus in the airways. This technique can be beneficial for individuals with conditions that cause excessive mucus production, such as cystic fibrosis. However, in the context of an acute asthma exacerbation, the primary concern is bronchoconstriction and inflammation, not mucus clearance. The child requires interventions that directly address airway constriction, such as bronchodilators. Therefore, while chest percussions may be helpful in certain situations, they are not the most appropriate intervention for managing acute asthma symptoms.
Choice D Reason: Have the child sit upright in a position of comfort
Having the child sit upright in a position of comfort can help improve breathing by allowing the lungs to expand more fully. This position can reduce the work of breathing and provide some relief from respiratory distress. While this intervention is supportive and can be beneficial, it is not sufficient on its own to manage an acute asthma exacerbation. The child requires pharmacological interventions, such as bronchodilators, to relieve bronchoconstriction and improve airflow. Therefore, while sitting upright is helpful, it should be combined with other interventions for optimal management of acute asthma symptoms.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
