A nurse on a mental health unit is caring for a client who is in restraints. Which of the following actions should the nurse take?
- Release the client's restraints every 4 hr.
- Check the client's status every hour.
- Document the client's behavior leading to the initiation of the restraints.
Obtain written consent by the client for the placement of the restraints.
Release the client's restraints every 4 hr.
Check the client's status every hour.
Document the client's behavior leading to the initiation of the restraints.
Obtain written consent by the client for the placement of the restraints.
The Correct Answer is C
Document the client's behavior leading to the initiation of the restraints: Accurate and comprehensive documentation is essential in the client's medical record. This includes documenting the client's behavior or actions that necessitated the use of restraints. It is important to document the reason, duration, and type of restraint used.
Release the client's restraints every 2 hours or as per institutional policy: It is important to periodically release the restraints to assess the client's circulation, skin integrity, and overall well-being. Restraints should never be kept on continuously without intermittent release. Check the client's status every 15 minutes: The nurse should closely monitor the client's vital signs, level of comfort, and any signs of distress or complications. Frequent assessment ensures early identification and intervention if any issues arise.
Obtain informed consent: While obtaining consent is necessary for many procedures or treatments, including the use of restraints, it is not applicable in situations where there is an imminent risk of harm to the client or others. The use of restraints in mental health units is based on legal and ethical guidelines, prioritizing the client's safety and the safety of others.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
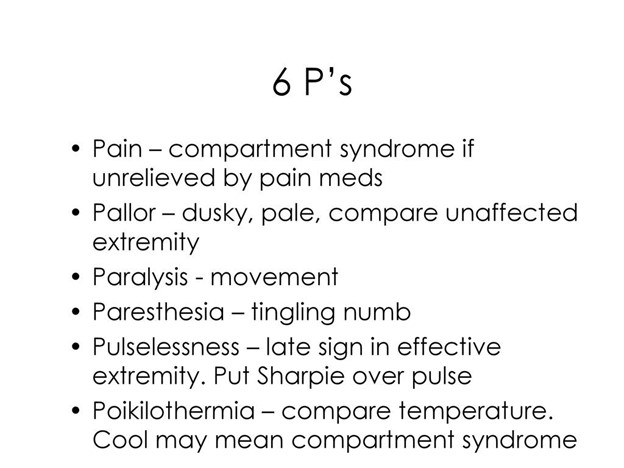
Diminished pulses in the affected extremity can indicate compromised circulation, which is a serious concern. It could suggest the development of compartment syndrome, a condition characterized by increased pressure within the muscles and tissues of the leg. Compartment syndrome can lead to tissue damage and potentially jeopardize the client's limb. Therefore, it is crucial for the nurse to recognize and address this finding promptly.
One fingerbreadth of space between the cast and the skin is generally considered an appropriate amount of space to allow for swelling and adequate circulation. However, it should still be monitored for any changes or signs of compartment syndrome.
Ecchymosis on the inner left thigh may indicate bruising, which could be related to the injury or the application of the cast. While it should be documented and monitored, it does not pose an immediate threat to the client's well-being.
Client report of muscle spasms of the left leg can be a common occurrence due to muscle immobility and discomfort associated with the cast. Although it should be assessed and managed for the client's comfort, it is not as urgent as addressing compromised circulation
Correct Answer is A
Explanation
Levothyroxine is a medication used to treat hypothyroidism, and monitoring the TSH levels helps determine the effectiveness of the medication.
Blood urea nitrogen (BUN) is a test used to assess kidney function and is not specifically related to thyroid function or levothyroxine therapy.
Prothrombin time (PT) is a test used to evaluate the clotting ability of the blood and is not directly related to thyroid function or levothyroxine therapy.
Arterial blood gases (ABGs) are used to assess oxygen and carbon dioxide levels in the blood and evaluate acid-base balance. ABGs are not specifically related to thyroid function or levothyroxine therapy.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
