The nurse is caring for a patient receiving a continuous norepinephrine (Levophed) IV infusion. Which patient assessment information indicates that the infusion rate may be too high?
Mean arterial pressure is 55 mm Hg.
Systemic vascular resistance (SVR) is elevated.
Pulmonary artery wedge pressure (PAWP) is low.
Heart rate is 58 beats/min.
The Correct Answer is D
Norepinephrine is a potent vasoconstrictor and inotropic agent commonly used to increase blood pressure in cases of hypotension or shock. However, if the infusion rate is too high, it can lead to excessive vasoconstriction and potentially compromise organ perfusion.
A heart rate of 58 beats/min suggests bradycardia, which can be an indication of excessive vasoconstriction caused by a high dose or rate of norepinephrine infusion. Excessive vasoconstriction can reduce cardiac output and worsen tissue perfusion.
A. Mean arterial pressure is 55 mm Hg in (option A) is incorrect because A mean arterial pressure of 55 mm Hg may be within an acceptable range for a patient receiving norepinephrine infusion, depending on the patient's baseline blood pressure and clinical condition.
B. Systemic vascular resistance (SVR) is elevated in (option B) is incorrect because An elevated SVR indicates increased peripheral vascular resistance and can be a desired effect of norepinephrine infusion to improve blood pressure and perfusion.
C. Pulmonary artery wedge pressure (PAWP) is low in (option C) which is incorrect because A low PAWP may indicate decreased left ventricular preload, which can be a desired effect of norepinephrine infusion to reduce fluid overload in certain clinical conditions.
It is important for the nurse to carefully monitor the patient's hemodynamic parameters, including blood pressure, heart rate, and organ perfusion when titrating norepinephrine infusion to ensure optimal dosing and minimize potential adverse effects. If concerns arise regarding the infusion rate, the healthcare provider should be promptly notified for further evaluation and adjustment of the treatment plan.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
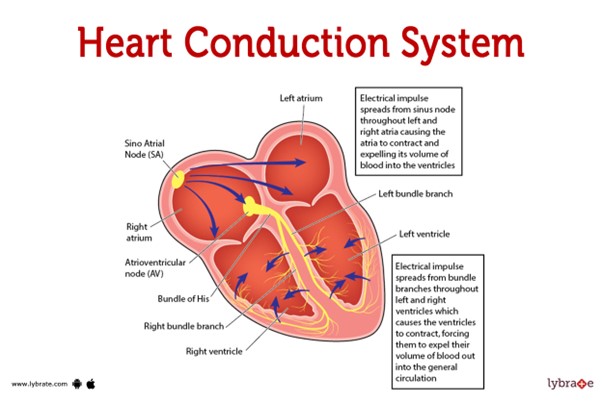 This pathway represents the normal sequence of electrical impulses that coordinate the contraction and relaxation of the heart chambers.
This pathway represents the normal sequence of electrical impulses that coordinate the contraction and relaxation of the heart chambers.
The electrical signal originates from the sinoatrial (SA) node, which is often referred to as the natural pacemaker of the heart. It is located in the right atrium and generates the electrical impulses that initiate each heartbeat. From the SA node, the electrical signal travels to the atrioventricular (AV) node, which is located at the junction between the atria and ventricles.
After passing through the AV node, the electrical impulse travels through the bundle of His (also known as the atrioventricular bundle) and divides into the right and left bundle branches. These branches continue the conduction pathway and deliver the electrical signal to the Purkinje fibers.
The Purkinje fibers spread the electrical impulse rapidly throughout the ventricles, stimulating the contraction of the ventricular muscle and allowing for efficient pumping of blood out of the heart.
Therefore, the correct sequence of the normal conduction pathway in the heart is:
A. SA node - AV node - bundle of His - bundle branches - Purkinje fibers.
Correct Answer is A
Explanation
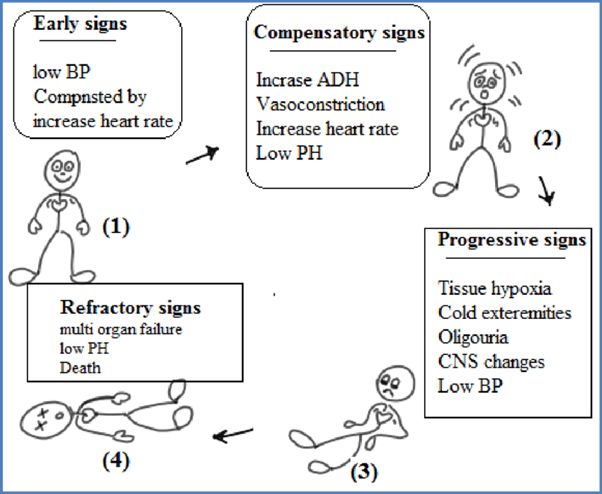
The stages of shock are commonly described as the initial, compensatory, progressive, and refractory stages. Here is an explanation of each stage and why the patient's assessment findings correspond to the progressive stage:
B. The compensatory stage in (option B) is incorrect because, In the compensatory stage, the body continues to activate compensatory mechanisms to maintain perfusion. This includes increased heart rate, peripheral vasoconstriction, and shunting of blood to vital organs. The patient's assessment findings of decreasing cardiac output, decreased peripheral perfusion, and increased capillary permeability suggest that the body's compensatory mechanisms are no longer sufficient to maintain perfusion adequately. Therefore, the patient has progressed beyond the compensatory stage.
C. The initial stage in (option C) is incorrect because, In the initial stage, there is an initial insult or injury that triggers the shock state. The body's compensatory mechanisms are activated, such as increased heart rate and vasoconstriction, to maintain blood pressure and perfusion. However, the patient's assessment findings indicate that they have progressed beyond the initial stage.
D. The refractory stage in (option D) is incorrect because The refractory stage represents a severe and irreversible state of shock where vital organs fail, and despite interventions, the patient's condition does not improve. The patient's assessment findings do not suggest the refractory stage, as there is still potential for intervention and management.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
