A nurse is caring for a client who is in a myxedema coma. Which of the following actions should the nurse take?
Place the client on aspiration precautions.
Turn the client every 4 hours.
Check the client’s blood pressure every 2 hours.
Initiate measures to cool the client.
The Correct Answer is A
Choice A Reason:
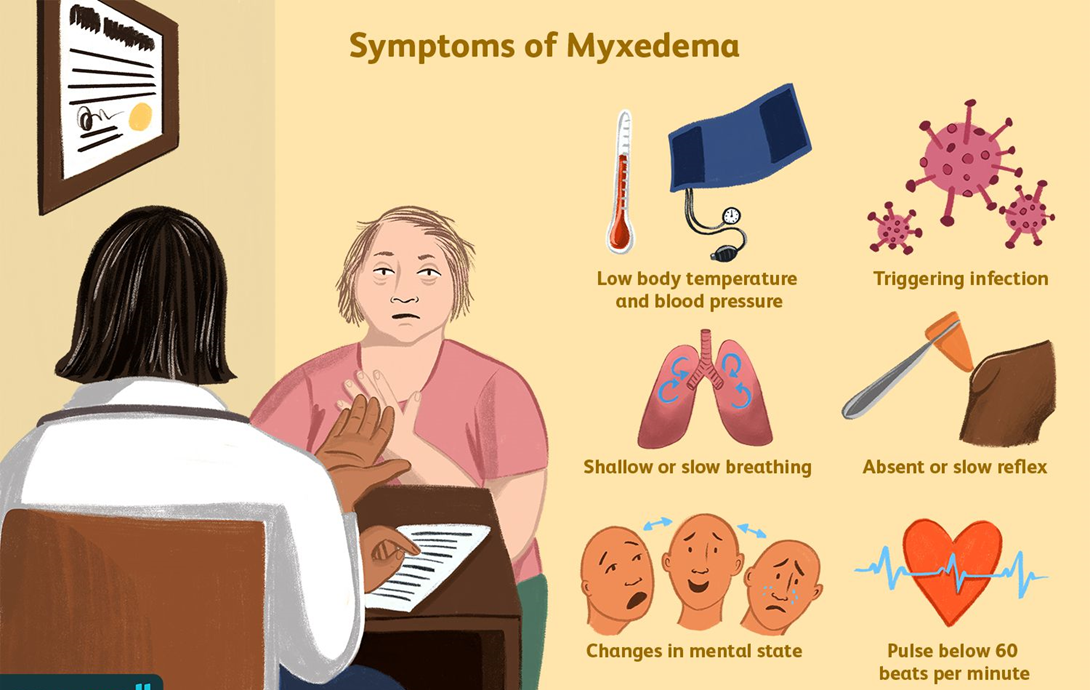
Place the client on aspiration precautions: Myxedema coma is a severe form of hypothyroidism that can lead to decreased mental function and a reduced level of consciousness. These conditions increase the risk of aspiration, which can lead to pneumonia and other complications. Therefore, placing the client on aspiration precautions is crucial to prevent these risks. Aspiration precautions may include elevating the head of the bed, monitoring swallowing ability, and providing thickened liquids if necessary.
Choice B Reason:
Turn the client every 4 hours: While turning the client regularly is important to prevent pressure ulcers, it is not the primary action needed for a client in a myxedema coma. The focus should be on stabilizing the client’s condition and preventing life-threatening complications such as aspiration, respiratory failure, and cardiovascular collapse.
Choice C Reason:
Check the client’s blood pressure every 2 hours: Monitoring vital signs, including blood pressure, is essential for clients in a myxedema coma. However, it is not the most critical action compared to preventing aspiration. Blood pressure should be monitored regularly, but the frequency can be adjusted based on the client’s condition and stability.
Choice D Reason:
Initiate measures to cool the client: Clients in a myxedema coma typically present with hypothermia (low body temperature), not hyperthermia (high body temperature). Therefore, initiating measures to cool the client would be inappropriate and could worsen their condition. Instead, measures to warm the client, such as using blankets and adjusting room temperature, are more appropriate.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A: You May Bring Some Music to Listen to for Distraction
Bringing music for distraction is generally not a standard instruction given before an EEG. While listening to music might help some patients relax, it is not a critical part of the preparation for the test. The primary focus of EEG preparation is to ensure accurate readings of brain activity, which can be influenced by various factors such as medication and sleep.
Choice B: Do Not Take Any Sedatives 12 to 24 Hours Before the Test
Avoiding sedatives before an EEG is crucial because these medications can alter brain activity and affect the test results. Sedatives can suppress the electrical activity in the brain, leading to inaccurate readings. Therefore, it is essential for patients to avoid taking any sedatives 12 to 24 hours before the test to ensure the EEG captures the brain’s natural activity.
Choice C: You Will Need to Have Someone to Drive You Home
This instruction is typically given if the patient is expected to be sedated or if the test involves procedures that might impair their ability to drive. However, for a standard EEG, patients are usually not sedated, and there is no need for someone to drive them home. This instruction is more relevant for other types of medical procedures that involve sedation.
Choice D: Please Do Not Have Anything to Eat or Drink After Midnight
Fasting is not a standard requirement for an EEG. Patients are generally allowed to eat and drink before the test. However, they are often advised to avoid caffeine as it can affect brain activity. The instruction to avoid food and drink after midnight is more commonly associated with procedures that require anesthesia or sedation, not an EEG.
Correct Answer is B
Explanation
Choice A Reason:
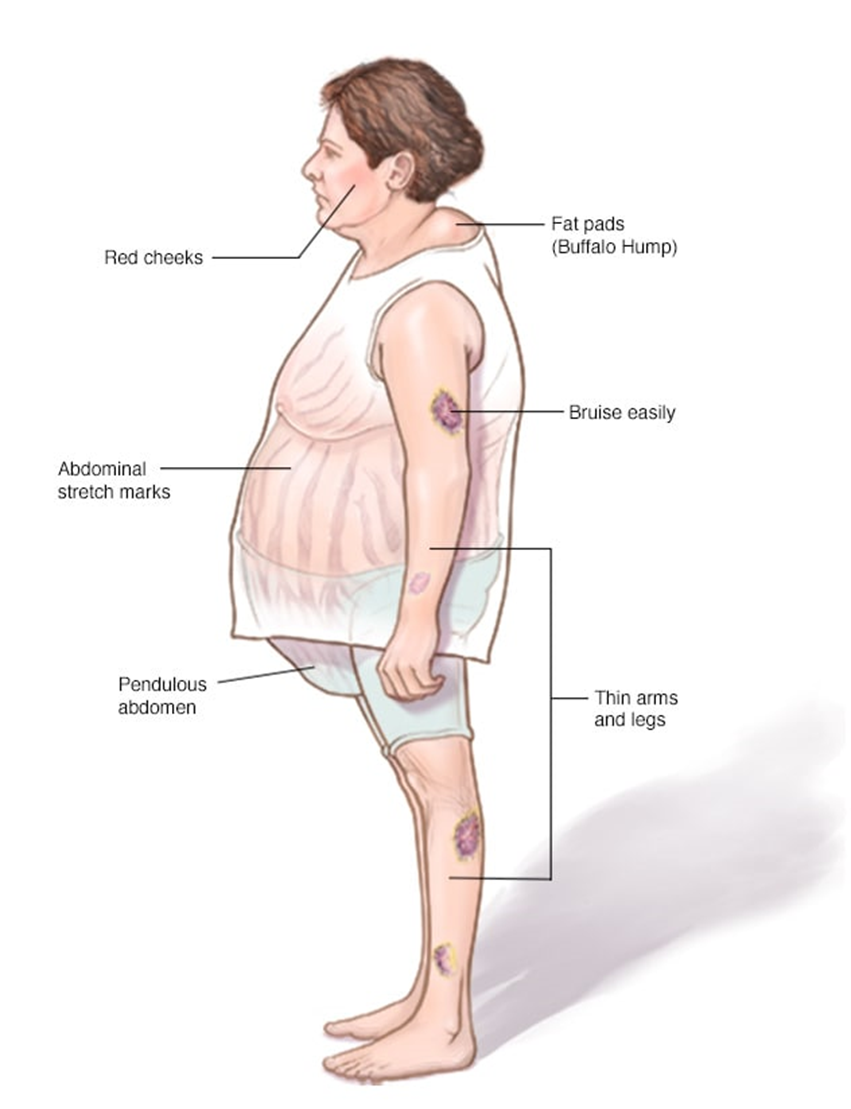
Decrease protein intake: This is not typically recommended for clients with Cushing’s disease. Protein is essential for maintaining muscle mass and overall health. Clients with Cushing’s disease often experience muscle weakness and wasting, so adequate protein intake is crucial to help counteract these effects. Therefore, decreasing protein intake would not be beneficial.
Choice B Reason:
Restrict sodium intake: Clients with Cushing’s disease often suffer from hypertension (high blood pressure) due to the excess cortisol in their bodies. High sodium intake can exacerbate this condition by increasing blood pressure even further. Therefore, it is crucial to restrict sodium intake to help manage hypertension and reduce the risk of cardiovascular complications. Foods high in sodium include processed foods, canned soups, and salty snacks. The recommended daily sodium intake for most adults is less than 2,300 milligrams, but for those with hypertension, it is often advised to consume even less.
Choice C Reason:
Limit intake of potassium-rich foods: This is not a standard recommendation for clients with Cushing’s disease. In fact, potassium is often beneficial as it can help counteract the effects of sodium and lower blood pressure. Potassium-rich foods include bananas, oranges, spinach, and sweet potatoes. Limiting these foods would not be advantageous and could potentially worsen hypertension.
Choice D Reason:
Increase carbohydrate intake: Increasing carbohydrate intake is not typically recommended for clients with Cushing’s disease. Excess cortisol can lead to increased blood sugar levels and a higher risk of developing diabetes. Therefore, it is important to manage carbohydrate intake carefully to avoid spikes in blood sugar. Instead, a balanced diet with a focus on complex carbohydrates, lean proteins, and healthy fats is recommended.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
