On admission to the emergency department, a patient with a C5 compression fracture can move only his head and has flaccid paralysis of all extremities. The distraught family asks if the paralysis is permanent. Which is the best response by the nurse?
"It is too early to tell. When the spinal shock subsides, we will know more."
"You should talk to your physician about things of that nature."
"No. Significant recovery of function should occur in a few days."
"Yes. In all likelihood, the paralysis is probably permanent."
The Correct Answer is A
A. "It is too early to tell. When the spinal shock subsides, we will know more."
This response is appropriate. Spinal shock can initially obscure the extent of neurological injury, and it may take time for the full extent of the injury to become apparent. By acknowledging this and suggesting that more information will be available once spinal shock subsides, the nurse provides a realistic perspective without prematurely predicting the outcome.
B. "You should talk to your physician about things of that nature."
This response may come across as dismissive or evasive. While it is true that the physician ultimately determines the patient's prognosis, the family may be seeking reassurance and guidance from the nurse as well.
C. "No. Significant recovery of function should occur in a few days."
This response is overly optimistic and potentially misleading. While some improvement may occur in the days following a spinal cord injury, significant recovery of function within a few days is unlikely, especially in cases of flaccid paralysis of all extremities.
D. "Yes. In all likelihood, the paralysis is probably permanent."
This response is overly pessimistic and lacks sensitivity. It may unnecessarily distress the family and extinguish hope for the patient's recovery.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","B","C","D","E","F"]
Explanation
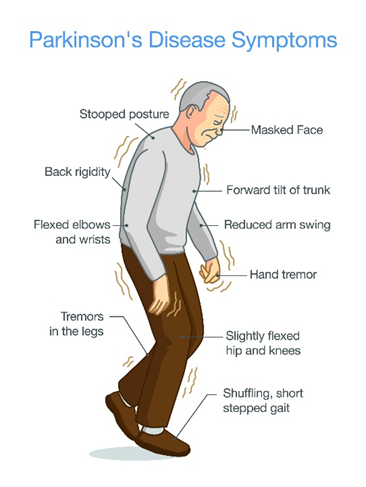
A. Muscle tremors:
Muscle tremors, particularly resting tremors, are a hallmark feature of Parkinson's disease. These tremors typically occur in the hands, fingers, arms, legs, jaw, or head and may worsen with stress or inactivity.
B. Slow body movement (bradykinesia):
Bradykinesia refers to slowness of movement and is another key symptom of Parkinson's disease. Patients may have difficulty initiating movement, experience a decrease in spontaneous movement (hypokinesia), and demonstrate reduced range of motion.
C. Rigidity:
Rigidity, or stiffness of the muscles, is a common symptom of Parkinson's disease. It often affects the limbs and trunk and can contribute to difficulty with movement and posture.
D. Pill rolling:
Pill rolling refers to a specific type of tremor characterized by rhythmic, rolling movements of the thumb and fingers, resembling the action of rolling a pill between the fingers and thumb. This tremor is commonly seen in Parkinson's disease.
E. Lack of facial expression:
Parkinson's disease can lead to a reduced range of facial expressions, also known as hypomimia or "masked facies." Patients may have a fixed, expressionless facial appearance and reduced blinking.
F. Drooling:
Drooling, or excessive salivation, can occur in Parkinson's disease due to impaired swallowing function (dysphagia) and reduced control over oral and facial muscles.
Correct Answer is B
Explanation
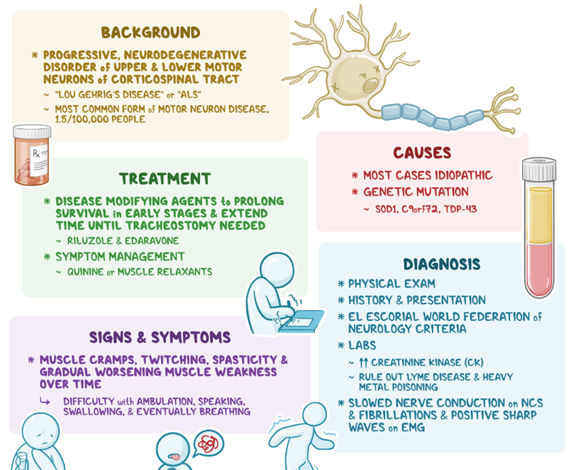
A. Intellectual capacity is not affected:
This statement refers to the fact that ALS primarily affects motor neurons, leading to muscle weakness and paralysis, but it typically does not directly impact cognitive function or intellectual capacity. While cognitive impairment is not a hallmark feature of ALS, some individuals may experience changes in cognitive function or behavior, such as executive dysfunction or frontotemporal dementia, in later stages of the disease. However, depression in ALS is not primarily linked to changes in intellectual capacity but rather to other factors such as altered communication, physical limitations, and loss of autonomy.
B. Communication is altered:
ALS can affect the muscles involved in speech and swallowing, leading to difficulties in communicationAs the disease progresses, patients may experience dysarthria (difficulty speaking clearly) and dysphagia (difficulty swallowing), which can impair their ability to communicate effectively with others. Altered communication can result in frustration, social isolation, and feelings of being misunderstood, all of which are risk factors for depression.
C. Mobility is limited:
ALS causes progressive muscle weakness and paralysis, which can significantly impair mobility over time. As the disease advances, individuals with ALS may become increasingly dependent on mobility aids such as wheelchairs or may require assistance with mobility tasks. Limited mobility can lead to feelings of loss of independence, decreased participation in activities, and increased dependence on caregivers, all of which can contribute to depression.
D. Nutritional intake is poor:
ALS can affect the muscles involved in swallowing and chewing, leading to difficulties with eating and drinking. Dysphagia, or difficulty swallowing, is a common symptom in ALS and can result in poor nutritional intake and weight loss. Malnutrition and weight loss are associated with increased morbidity and mortality in ALS, and they can also contribute to feelings of weakness, fatigue, and overall decline in quality of life, which may exacerbate depression.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
