The nurse takes a client's temperature before giving a blood transfusion. The temperature is 100 F orally. The nurse reports the finding to the registered nurse (RN) and anticipates that which action will take place?
The transfusion will begin after the administration of 650 mg of acetaminophen {Tylenol).
The blood will be held, and the health care provider will be notified
The transfusion will begin after the administration of an antihistamine
The transfusion will begin as prescribed
The Correct Answer is A
A. The transfusion will begin after the administration of 650 mg of acetaminophen (Tylenol).
This option suggests that the nurse would administer acetaminophen to lower the client's temperature and then proceed with the blood transfusion. While acetaminophen can be used to reduce fever, the decision to administer medication should be made by the healthcare provider after assessing the client's overall condition and determining the cause of the fever. Administering medication without proper evaluation and orders from the healthcare provider is not appropriate.
B. The blood will be held, and the health care provider will be notified.
This option is the correct choice. When a client has an elevated temperature before a blood transfusion, it is standard practice to hold the transfusion and notify the healthcare provider. An elevated temperature could indicate an underlying infection or another condition that needs to be evaluated before proceeding with the transfusion to ensure the client's safety.
C. The transfusion will begin after the administration of an antihistamine.
Administering an antihistamine would not be the appropriate action in response to an elevated temperature before a blood transfusion. Antihistamines are typically used to treat allergic reactions, not fevers. Holding the transfusion and notifying the healthcare provider to assess the situation would be the correct course of action.
D. The transfusion will begin as prescribed.
This option is not appropriate because starting the transfusion without addressing the elevated temperature could pose risks to the client's health. Elevated temperatures may indicate an underlying infection or other conditions that need to be evaluated before proceeding with the transfusion. Holding the transfusion and seeking further guidance from the healthcare provider is the recommended action in this scenario.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
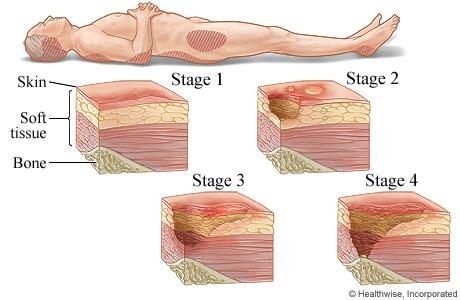
A. Stage III pressure injury
Stage III pressure injuries involve full-thickness skin loss, extending into the subcutaneous tissue but not through the fascia. These wounds typically present as deep craters and may involve undermining or tunneling. Non-blanchable erythema alone without visible skin loss is not characteristic of a Stage III pressure injury.
B. Stage IV pressure injury
Stage IV pressure injuries are the most severe and involve full-thickness tissue loss with exposed bone, tendon, or muscle. These wounds often have extensive tissue damage and can be difficult to manage. Again, non-blanchable erythema without visible skin loss is not indicative of a Stage IV pressure injury.
C. Stage II pressure injury
Stage II pressure injuries involve partial-thickness skin loss with damage to the epidermis and possibly the dermis. These wounds often present as shallow open ulcers or blisters and may have characteristics such as intact or ruptured blisters. While Stage II injuries can present with erythema, non-blanchable erythema specifically indicates a Stage I injury.
D. Stage I pressure injury
Stage I pressure injuries are the earliest stage and involve non-blanchable erythema of intact skin. The skin may be warmer or cooler than surrounding tissue and may have changes in sensation. There is no visible skin loss at this stage, but the area is at risk for further injury if pressure is not relieved. Therefore, non-blanchable erythema on the heels most likely indicates a Stage I pressure injury.
Correct Answer is B
Explanation
A. Melanoma:
Melanoma is a type of skin cancer that arises from melanocytes, the cells that produce pigment (melanin) in the skin. Melanoma lesions are typically irregularly shaped, often asymmetrical, with varying shades of color (brown, black, tan, red, blue). They may have an uneven border and can evolve over time. Melanomas can be raised but are not typically described as indurated (firm) and shiny. They are also more commonly associated with changes in color, size, and shape.
B. Keloid:
A keloid is an abnormal overgrowth of scar tissue that extends beyond the boundaries of the original wound or incision site. Keloids are characterized by their raised appearance, firm or indurated texture, and shiny surface compared to the surrounding skin. They may also be darker than the surrounding skin due to increased collagen deposition. Keloids can develop months after an injury or surgery and are more common in individuals with darker skin tones, such as African Americans.
C. Nevus:
A nevus, commonly known as a mole or birthmark, is a benign growth of melanocytes or other skin cells. Nevus lesions can vary in appearance but are often flat or slightly raised, with a uniform color (brown, black, tan, or flesh-colored). They are usually not described as indurated or shiny. Nevus lesions can be present at birth (congenital nevus) or develop later in life (acquired nevus).
D. Angioma:
Angiomas are benign tumors that originate from blood vessels or lymphatic vessels. They can present as red or purplish raised lesions on the skin. Angiomas are typically not described as indurated or shiny. Common types of angiomas include cherry angiomas (small, red papules) and spider angiomas (red, spider-like lesions with central vessels).
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
