The nurse, working in labor and delivery, performs a sterile vaginal exam on a laboring woman. During the exam, she feels a loop of pulsating cord in the vagina. The nurse would anticipate:
Select one:
Continuing to monitor and document fetal heart rate.
Changing the mother's position to left lateral and giving oxygen by nasal cannula.
With a sterile glove, maintaining pressure to lift the presenting part and emergently notifying the provider for a STAT C-section.
Bolusing the patient with 1000cc lactated ringers
The Correct Answer is C
Choice A Reason: Continuing to monitor and document fetal heart rate. This is an inadequate response that does not address the urgency of the situation or intervene to prevent fetal distress or demise.
Choice B Reason: Changing the mother's position to left lateral and giving oxygen by nasal cannula. This is a partial response that may improve maternal-fetal blood flow and oxygenation, but it does not resolve the cord compression or facilitate delivery.
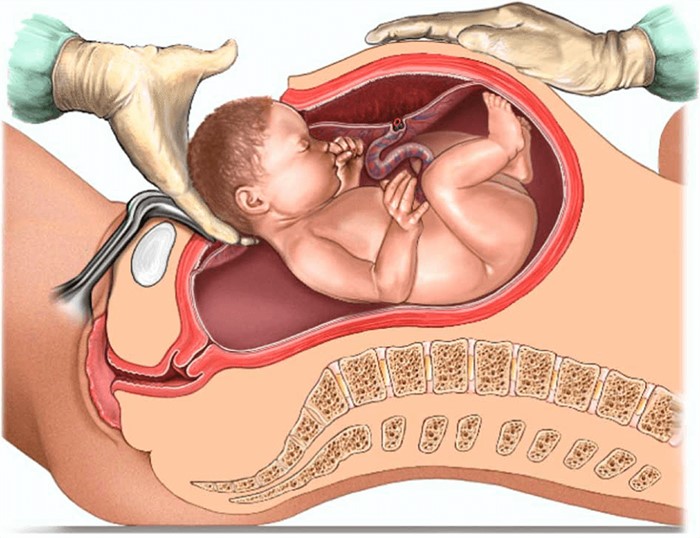
Choice C Reason: With a sterile glove, maintaining pressure to lift the presenting part and emergently notifying the provider for a STAT C-section. This is an appropriate response that aims to reduce the cord compression by elevating the fetal head away from the cord and prepare for an immediate cesarean delivery.
Choice D Reason: Bolusing the patient with 1000cc lactated ringers. This is an irrelevant response that does not address the cause of the problem or improve fetal outcome.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A Reason: "Your body is responding to the events of labor, just like after a tough workout." This is an inaccurate statement that does not explain the cause of the contractions or reassure the client.
Choice B Reason: "This could be a sign that your body is trying to get rid of retained placental fragments." This is an alarming statement that may scare the client and imply that something is wrong. Retained placental fragments are rare and usually cause heavy bleeding, fever, and infection.
Choice C Reason: "Let me check your vaginal discharge just to make sure everything is fine." This is an unnecessary statement that does not answer the client's question or provide any information.
Choice D Reason:"The baby's sucking releases oxytocin which causes your uterus to contract." This is a correct statement that explains the physiological mechanism of the contractions and reassures the client that they are normal and beneficial.
Correct Answer is D
Explanation
Choice A Reason: Preterm infant. This is an incorrect answer that confuses TTN with another respiratory condition called respiratory distress syndrome (RDS). RDS is a serious condition where the newborn's lungs are immature and lack sufficient surfactant, which is a substance that reduces surface tension and prevents alveolar collapse. RDS can cause respiratory distress, hypoxia, acidosis, and organ failure. It is more common in preterm infants, especially those born before 37 weeks' gestation.
Choice B Reason: Female infant. This is an incorrect answer that has no evidence or rationale to support it. TTN does not have a gender preference or difference in incidence or severity.
Choice C Reason: GBS status of mother. This is an incorrect answer that relates to another respiratory complication called early-onset neonatal sepsis (EONS). EONS is a bacterial infection that occurs within 72 hours after birth, which can affect multiple organs and systems in the newborn. EONS can be caused by group B streptococcus (GBS), which is a common bacterium that colonizes in some women's vagina or rectum. GBS can be transmited to the newborn during delivery and cause pneumonia, meningitis, or septic shock.
Choice D Reason: Cesarean section. This is because cesarean section is a risk factor for TTN, which is a mild respiratory problem that results from delayed clearance of fetal lung fluid after birth. TTN causes rapid breathing, nasal flaring, grunting, and mild cyanosis. It usually resolves within 24 to 48 hours after birth. Cesarean section can increase the risk of TTN because it bypasses the normal process of labor, which helps squeeze out some of the fluid from the fetal lungs.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
