Pharmacologic Pain Management During Labor
Pharmacologic pain management methods are techniques that involve medications or invasive procedures to relieve pain during labor. They aim to reduce pain intensity, modify pain perception, or block pain transmission.
Some of the benefits of pharmacologic methods are that they provide effective, consistent, and predictable pain relief for most women, they do not require active participation from the woman or her support person, and they can be adjusted according to the woman’s needs.
Some of the limitations are that they may have adverse effects on the mother or the fetus, they may interfere with maternal-fetal bonding, they may require additional monitoring or interventions, and they may not be available or acceptable in some cultures or settings.
Some examples of pharmacologic pain management methods are:
Systemic analgesics: These are medications that are administered orally, intramuscularly, or intravenously to provide sedation, anxiolysis, and analgesia during labor.
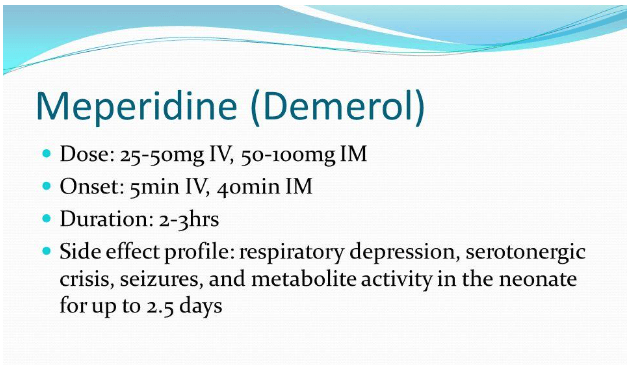
Systemic analgesics include opioids (such as meperidine, fentanyl, or morphine), antiemetics (such as promethazine), and benzodiazepines (such as diazepam).
Systemic analgesics provide pain relief that is superior to nitrous oxide but inferior to regional anesthesia.
Systemic analgesics can also reduce anxiety, nausea, vomiting, and shivering during labor.
However, systemic analgesics may cause maternal respiratory depression, hypotension, drowsiness, confusion, or pruritus.
Systemic analgesics may also cross the placenta and cause fetal respiratory depression, bradycardia, decreased variability, or neurobehavioral changes.
Systemic analgesics should be used with caution in women with asthma, cardiac disease, renal disease, liver disease, or opioid use disorder.
Systemic analgesics should also be timed carefully to avoid peak effects at delivery.
-
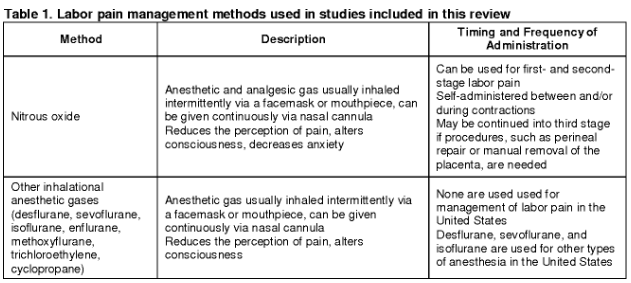
Inhaled analgesia: This is a method that involves inhaling a mixture of nitrous oxide (N2O) and oxygen (O2) through a mask or mouthpiece to provide self-administered analgesia during labor.
Inhaled analgesia provides mild to moderate pain relief that is comparable to parenteral opioids but less than regional anesthesia.
Inhaled analgesia can also reduce anxiety, nausea, vomiting, and shivering during labor.
However, inhaled analgesia may cause maternal dizziness, headache, drowsiness, nausea, vomiting, or dry mouth.
Inhaled analgesia may also have negative environmental impact as a greenhouse gas.
Inhaled analgesia should be used with caution in women with vitamin B12 deficiency, pulmonary disease, bowel obstruction, or pneumothorax.
Inhaled analgesia should also be discontinued at least 30 minutes before delivery to avoid neonatal depression.
Regional anesthesia: This is a method that involves injecting local anesthetics into specific regions of the body to block nerve impulses from reaching the brain.
Regional anesthesia provides the most effective pharmacologic analgesia during labor and is used in nearly three-fourths of labors in the United States.
Regional anesthesia can also reduce stress hormones, blood pressure, cardiac workload, and blood loss during labor.
However, regional anesthesia may cause maternal hypotension, bradycardia, fever, itching, urinary retention, or headache.
Regional anesthesia may also prolong the second stage of labor, increase the need for oxytocin augmentation or instrumental delivery, or interfere with maternal-fetal bonding.
Regional anesthesia should be performed by an anesthesiologist or a certified registered nurse anesthetist under strict aseptic technique.
Regional anesthesia should also be accompanied by adequate hydration, monitoring of vital signs and fetal heart rate, and prevention of supine hypotension syndrome by placing a wedge under the right hip.
Some examples of regional anesthesia techniques are:
-
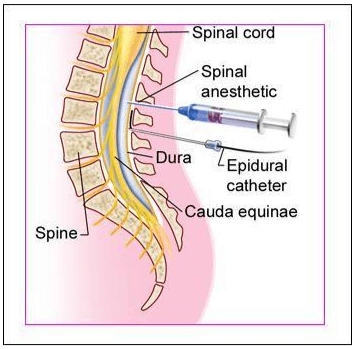
Epidural anesthesia: This involves placing a small catheter into the epidural space between L3-L4 or L4-L5 vertebrae through which local anesthetics (such as bupivacaine) and opioids (such as fentanyl) are administered continuously or intermittently.
Epidural anesthesia provides lack of sensation from the level at umbilicus to thighs.
Epidural anesthesia requires at least 4 cm of cervical dilation before insertion.
-
Spinal anesthesia: This involves injecting local anesthetics (such as bupivacaine) and opioids (such as fentanyl) into the subarachnoid space between L3-L4 or L4-L5 vertebrae through which local anesthetics (such as bupivacaine) and opioids (such as fentanyl) are injected once or twice.
Spinal anesthesia provides lack of sensation from the nipples to the feet.
Spinal anesthesia is used mainly for cesarean delivery or forceps delivery.
-
Combined spinal-epidural (CSE) anesthesia: This involves placing a small catheter into the epidural space and then injecting local anesthetics and opioids into the subarachnoid space through a needle that passes through the catheter.
CSE anesthesia combines the advantages of both epidural and spinal anesthesia, such as rapid onset, dense block, and prolonged duration.
CSE anesthesia can also provide better sacral coverage and less motor block than epidural or spinal anesthesia alone.
-
Dural puncture epidural (DPE) anesthesia: This involves placing a small catheter into the epidural space and then intentionally puncturing the dura mater with a needle to create a small hole.
DPE anesthesia allows cerebrospinal fluid to leak into the epidural space, which enhances the spread and effectiveness of local anesthetics administered through the catheter.
DPE anesthesia can provide faster onset, lower dose requirement, and better sacral coverage than epidural anesthesia alone.
-
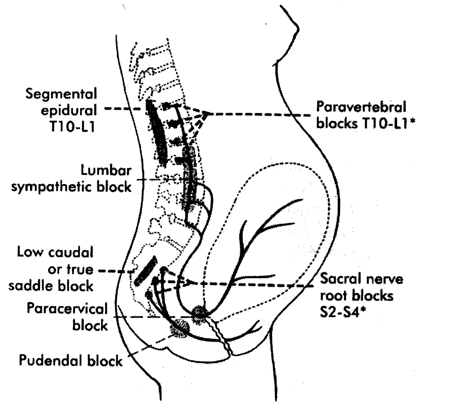
Paracervical block: This involves injecting local anesthetics (such as lidocaine) into the paracervical area at 3 o’clock and 9 o’clock positions.
Paracervical block provides lack of sensation from the cervix to the lower vagina.
Paracervical block is used mainly for pain relief during the first stage of labor or for cervical dilation before instrumental delivery.
-
Pudendal block: This involves injecting local anesthetics (such as lidocaine) into the pudendal nerve near the ischial spine on both sides.
Pudendal block provides lack of sensation from the lower vagina to the perineum.
Pudendal block is used mainly for pain relief during the second stage of labor or for episiotomy repair.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Questions on Pharmacologic Pain Management During Labor
Correct Answer is B
Explanation
Correct Answer is B
Explanation
Correct Answer is B
Explanation
Correct Answer is D
Explanation
Correct Answer is A
Explanation
Search Here
More on Nursing
- Newborn Complications
- Physiological And Physical Changes In Pregnancy
- Prenatal Diagnostic Tests And Procedures
- Pre-eclampsia, Eclampsia
- Pre-term Labor
- Contraception
- Prolonged and Obstructed Labor and Ruptured Uterus
- Phases of Maternal Role Attainment
- Postpartum Depression
- Postpartum Disorders: DVT, Pulmonary Embolism
Free Nursing Study Materials
Access to all study guides and practice questions for nursing for free.
- Free Nursing Study Trials
- Free Nursing Video tutorials
- Free Nursing Practice Tests
- Free Exam and Study Modes
- Free Nursing Revision Quizlets
