Med Surg Final Exam
ATI Med Surg Final Exam
Total Questions : 41
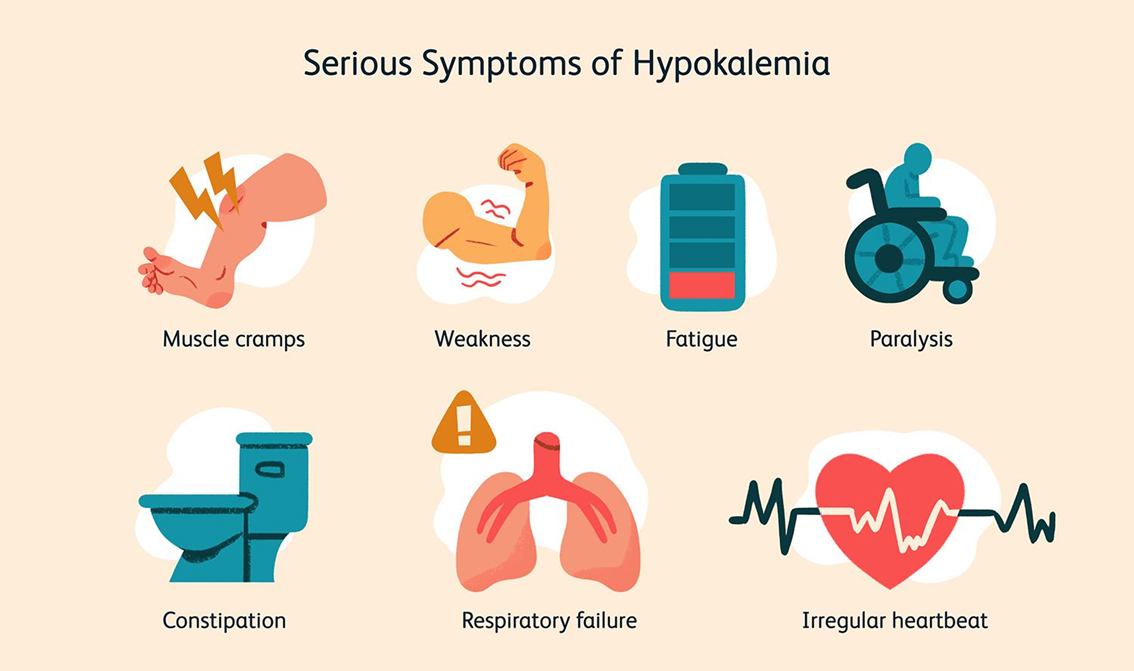
Showing 10 questions Sign up for moreA nurse is providing care for a client with hypokalemia. Which condition should the nurse monitor for?
Explanation
Choice A reason: Hypertension is not directly caused by hypokalemia. While potassium levels can influence blood pressure, hypokalemia is more critically associated with cardiac issues rather than hypertension alone.
Choice B reason: Ketosis is a metabolic state resulting from the body burning fat for fuel instead of carbohydrates. It is not directly related to hypokalemia. Hypokalemia does not cause ketosis, and monitoring for ketosis in a client with hypokalemia is not a priority.
Choice C reason: Insulin resistance is a condition where the body’s cells do not respond properly to insulin. While potassium levels can affect insulin secretion and action, hypokalemia is not primarily associated with insulin resistance. Therefore, it is not the main concern for a nurse monitoring a client with hypokalemia.
Choice D reason: Cardiac arrhythmias are a significant concern in clients with hypokalemia. Potassium is crucial for proper cardiac function, and low levels can lead to abnormal heart rhythms. This is why monitoring for cardiac arrhythmias is essential in clients with hypokalemia.
Explanation
Choice A Reason:
This statement is incorrect because a hemoglobin A1C level of 9% indicates that the client’s blood sugar levels have been consistently high over the past two to three months. Hemoglobin A1C is a measure of average blood glucose levels, not low blood sugar levels. Therefore, it would be inappropriate to suggest that the client has dangerously low blood sugar levels based on this result.
Choice B Reason:
This statement is correct because a hemoglobin A1C level of 9% indicates that the client’s average blood sugar levels are high. Hemoglobin A1C reflects the average blood glucose levels over the past two to three months. A normal A1C level is below 5.7%, while an A1C level between 5.7% and 6.4% indicates prediabetes, and an A1C level of 6.5% or higher indicates diabetes. Therefore, an A1C level of 9% clearly shows that the client’s average blood sugar is high.
Choice C Reason:
This statement is partially correct but not the most appropriate. While it is true that a high hemoglobin A1C level can indicate that blood sugar levels are high after meals, it is not specific enough. Hemoglobin A1C measures the average blood glucose levels over a period of time, not just after meals. Therefore, the statement “Your average blood sugar is high” is more accurate and appropriate.
Choice D Reason:
This statement is incorrect because it is too vague and does not provide specific information about the client’s blood sugar levels. While a high hemoglobin A1C level can indicate variability in blood sugar levels, it primarily reflects the average blood glucose levels over the past two to three months. Therefore, it would be more appropriate to state that the client’s average blood sugar is high.
The nurse is caring for a patient with type 2 diabetes mellitus who has been prescribed doses of insulin.
Explanation
Choice A Reason:
Monitoring blood glucose levels is crucial for managing diabetes, but in the context of hyperosmolar hyperglycemic syndrome (HHS), recognizing the signs and symptoms is more critical. HHS is a serious condition characterized by extremely high blood sugar levels without significant ketoacidosis. Early recognition of symptoms such as extreme thirst, frequent urination, confusion, and weakness can prevent complications and prompt timely medical intervention.
Choice B Reason:
Recognizing signs and symptoms of HHS is the most important topic to prioritize. HHS can develop gradually and may be life-threatening if not identified and treated promptly. Patients and caregivers need to be aware of the warning signs to seek immediate medical attention. Symptoms include severe dehydration, altered mental status, and very high blood glucose levels. Educating patients on these signs ensures they can act quickly to prevent severe outcomes.
Choice C Reason:
Administering insulin correctly is essential for managing diabetes, but it is not the top priority in the context of HHS education. While proper insulin administration helps control blood glucose levels, the immediate concern in HHS is recognizing the condition’s onset. Once HHS is identified, insulin administration becomes part of the treatment plan, but early detection is key to preventing severe complications.
Choice D Reason:
Understanding the importance of hydration is important because dehydration is a significant component of HHS. Patients with HHS often experience severe dehydration due to high blood glucose levels leading to osmotic diuresis. Educating patients on maintaining adequate hydration can help manage their condition and prevent the onset of HHS. However, recognizing the symptoms of HHS remains the top priority.
Choice E Reason:
Managing diet and nutrition is a fundamental aspect of diabetes care, but it is not the primary focus when dealing with HHS. While a balanced diet helps maintain stable blood glucose levels, the immediate concern in HHS is identifying and responding to the condition’s symptoms. Once HHS is recognized and treated, dietary management becomes part of the long-term care plan.
A nurse is caring for a client who was diagnosed with type 2 diabetes mellitus 2 years ago. The client reports following the recommended diet and exercising four times per week. Which of the following findings indicates that the client’s beta cells are restoring normal function?
Explanation
Choice A: Fasting blood glucose of 140 mg/dL
A fasting blood glucose level of 140 mg/dL is above the normal range (70-99 mg/dL) but may indicate some improvement in beta cell function if it was previously higher. In type 2 diabetes, beta cells in the pancreas are responsible for producing insulin. When beta cells start to restore their function, they can produce more insulin, which helps lower blood glucose levels. However, a fasting blood glucose level of 140 mg/dL still indicates that the client has diabetes and needs to continue managing their condition.
Choice B: Client reports smoking cessation
Smoking cessation is a positive health behavior and can improve overall health, including cardiovascular health, which is often compromised in individuals with diabetes. However, it does not directly indicate the restoration of beta cell function. Beta cell function is specifically related to the pancreas’s ability to produce insulin, and smoking cessation, while beneficial, does not directly impact this.
Choice C: Weight gain of 5 lb
Weight gain can have various implications for a person with type 2 diabetes. While modest weight gain might indicate improved nutritional status or muscle mass, it does not directly indicate the restoration of beta cell function. In fact, weight gain can sometimes worsen insulin resistance, making it harder for beta cells to function effectively.
Explanation
Choice A reason:
A client admitted for hip fracture surgery is at risk for various complications, but not specifically for hyperosmolar hyperglycemic syndrome (HHS). HHS is more commonly triggered by infections, severe dehydration, or other acute illnesses. While surgery can be a stressor, it is not as directly linked to HHS as infections are.
Choice B reason:
A client who is awaiting cataract surgery is not typically at high risk for developing HHS. Cataract surgery is generally a planned and controlled procedure that does not usually involve the acute stressors or infections that can precipitate HHS.
Choice C reason:
A client who is receiving an antibiotic for a urinary tract infection is at a higher risk for developing HHS. Infections are a common precipitating factor for HHS because they can cause significant stress on the body, leading to elevated blood glucose levels. The body’s response to infection can exacerbate hyperglycemia, especially in individuals with type 2 diabetes.
Choice D reason:
A client who is being evaluated for a breast lump is not typically at high risk for HHS. While the evaluation process can be stressful, it does not usually involve the acute physiological stressors or infections that are more directly linked to the development of HHS.
Explanation
Choice A Reason:
Dietary and fluid restrictions are crucial for managing heart failure. Patients with heart failure often experience fluid retention, which can exacerbate symptoms such as swelling, shortness of breath, and fatigue. By restricting fluid intake, patients can help prevent fluid overload. Additionally, dietary modifications, such as reducing sodium intake, can help manage blood pressure and reduce the risk of fluid retention. Sodium causes the body to retain water, which can increase the workload on the heart. Therefore, a low-sodium diet is often recommended for heart failure patients. These restrictions are essential to prevent the worsening of heart failure symptoms and to improve the patient’s quality of life.
Choice B Reason:
Encouraging increased mobility is generally beneficial for overall health, but it must be approached cautiously in heart failure patients. While regular physical activity can help improve cardiovascular health and overall well-being, it is important to tailor the exercise regimen to the patient’s condition. Overexertion can lead to worsening symptoms or complications. Therefore, while increased mobility can be part of the management plan, it should be done under medical supervision and is not the primary lifestyle modification for heart failure management.
Choice C Reason:
Cessation of hormonal supplements may be relevant for some patients, particularly if the supplements are contributing to fluid retention or other adverse effects. However, this is not a standard recommendation for all heart failure patients. The decision to stop hormonal supplements would depend on the individual patient’s medical history and the specific supplements they are taking. It is not a general lifestyle modification for heart failure management.
Choice D Reason:
Cessation of intravenous (IV) drug use is important for patients who may be using IV drugs, as this can lead to infections, endocarditis, and other complications that can worsen heart failure. However, this recommendation is specific to patients with a history of IV drug use and is not a general lifestyle modification for all heart failure patients. The primary focus for most heart failure patients would be on managing fluid and dietary intake.
A nurse is providing discharge teaching to a client who has heart failure. Which of the following lifestyle modifications should the nurse include in the discharge teaching?
Explanation
Choice A: Dietary and Fluid Restrictions
Dietary and fluid restrictions are crucial for patients with heart failure. These restrictions help manage symptoms and prevent complications. Limiting sodium intake can reduce fluid retention, which decreases the workload on the heart. Fluid restrictions help prevent fluid overload, which can lead to worsening heart failure symptoms. Patients are often advised to monitor their weight daily to detect fluid retention early. This choice is essential for managing heart failure effectively.
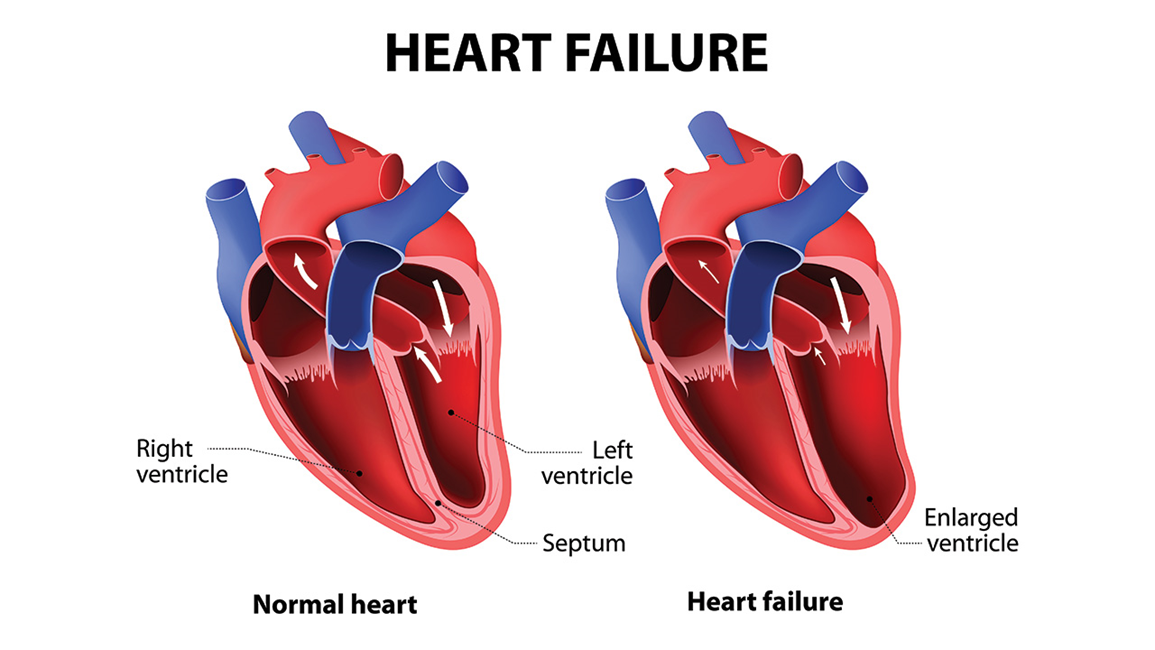
Choice B: Encouraging Increased Mobility
While physical activity is generally beneficial for overall health, it must be approached cautiously in patients with heart failure. Encouraging increased mobility without proper medical guidance can lead to overexertion and exacerbate heart failure symptoms. Exercise programs for heart failure patients should be tailored and supervised by healthcare professionals to ensure safety and effectiveness. Therefore, this choice is not as immediately critical as dietary and fluid restrictions.
Choice C: Cessation of Hormonal Supplements
Hormonal supplements can have various effects on the cardiovascular system, but their cessation is not a standard recommendation for all heart failure patients. The impact of hormonal supplements depends on the specific type and the patient’s overall health condition. This choice is less relevant compared to dietary and fluid restrictions, which have a direct and significant impact on heart failure management.
Choice D: Cessation of Intravenous (IV) Drug Use
Cessation of intravenous drug use is important for overall health and preventing infections, but it is not specific to heart failure management. While IV drug use can lead to complications that may affect the heart, it is not a primary lifestyle modification recommended for heart failure patients. The focus should be on managing fluid balance and dietary intake
Explanation
Choice A reason: Metabolic alkalosis is a condition characterized by an elevated pH in body tissues, typically due to an excess of bicarbonate or a loss of hydrogen ions. This condition is not associated with Kussmaul breathing. Kussmaul breathing is a deep and labored breathing pattern often seen in patients with metabolic acidosis, not alkalosis. In metabolic alkalosis, the body does not need to expel excess acid through rapid breathing, so Kussmaul respirations are not observed.
Choice B reason: Metabolic acidosis is a condition where there is an excess of acid in the body due to the accumulation of acid or the loss of bicarbonate. This condition is commonly seen in diabetic ketoacidosis (DKA), where the body produces high levels of ketones, leading to acidosis. Kussmaul breathing is a compensatory mechanism in metabolic acidosis, where the body attempts to reduce the acid level by expelling carbon dioxide through rapid, deep breaths. This type of breathing helps to lower the blood’s acidity by reducing the concentration of carbon dioxide, which is an acid.
Choice C reason: Respiratory alkalosis is a condition where there is a decrease in carbon dioxide levels in the blood due to excessive breathing or hyperventilation. This condition leads to an increase in blood pH, making it more alkaline. Kussmaul breathing is not associated with respiratory alkalosis because it is a response to metabolic acidosis, not a condition where the body is already expelling too much carbon dioxide.
Choice D reason: Respiratory acidosis is a condition where there is an excess of carbon dioxide in the blood due to inadequate respiration. This leads to a decrease in blood pH, making it more acidic. While respiratory acidosis involves an acidic environment, Kussmaul breathing is specifically a response to metabolic acidosis, not respiratory acidosis. In respiratory acidosis, the body would not use Kussmaul respirations as a compensatory mechanism.
Explanation
Choice A Reason:
Coronary arteries do not become more elastic with age. Instead, they tend to become less elastic due to the buildup of plaque, a condition known as atherosclerosis. This buildup narrows the arteries and restricts blood flow, which can lead to coronary artery disease (CAD). The heart not receiving enough oxygen is a result of this narrowing, not increased elasticity.
Choice B Reason:
Coronary arteries decrease in diameter due to the buildup of plaque, which consists of fats, cholesterol, and other substances. This narrowing restricts the flow of blood, oxygen, and nutrients to the heart muscle, leading to symptoms such as chest pain (angina) and shortness of breath. This is the primary mechanism behind coronary artery disease.
Choice C Reason:
This choice is essentially a repetition of Choice B and is correct for the same reasons. The narrowing of the coronary arteries due to plaque buildup leads to insufficient blood flow, causing the heart muscle to receive less oxygen and nutrients.
Choice D Reason:
Manifestations of coronary artery disease are not due to the dilation of coronary arteries. Instead, they are due to the narrowing of these arteries. Increased blood flow and pressure are not typical causes of CAD symptoms. The primary issue is the restricted blood flow due to narrowed arteries.
Choice E Reason:
While it is true that the heart and coronary arteries can weaken over time, leading to poor perfusion and angina, this statement does not accurately describe the primary mechanism of coronary artery disease. The main issue in CAD is the narrowing of the arteries due to plaque buildup, which restricts blood flow to the heart muscle.
A nurse is assessing a client who has peripheral venous disease. Which of the following findings should the nurse recognize as a manifestation of venous disease?
Explanation
Choice A Reason:
Swollen and enlarged veins, also known as varicose veins, are a common manifestation of peripheral venous disease (PVD). This condition occurs when the valves in the veins become weak or damaged, leading to blood pooling and increased pressure within the veins. This results in the veins becoming enlarged, twisted, and visible under the skin1. Varicose veins can cause discomfort, pain, and a heavy feeling in the legs. They are often exacerbated by prolonged standing or sitting and can be a cosmetic concern as well.
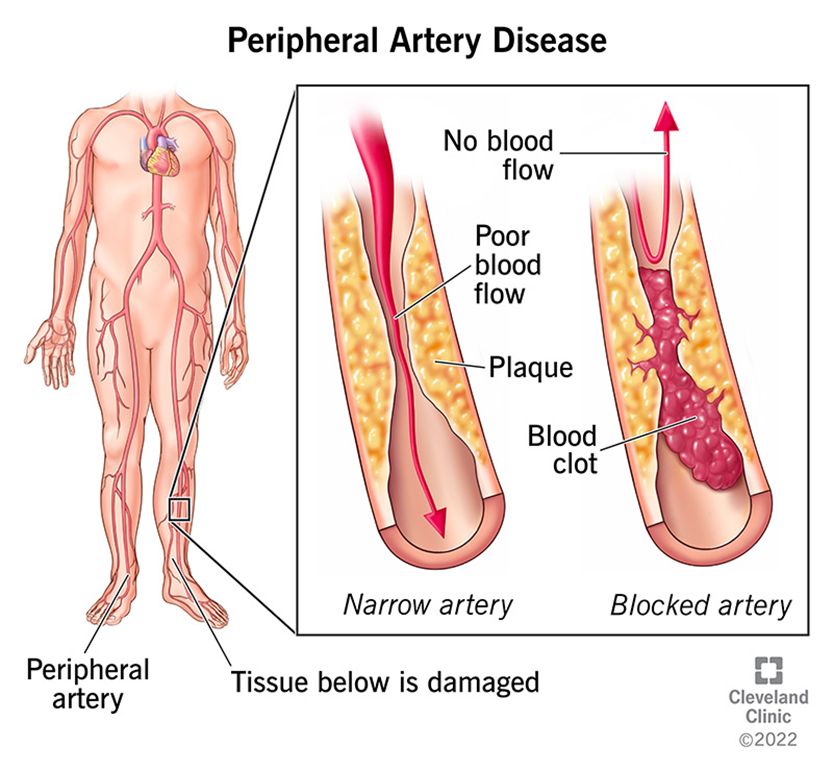
Choice B Reason:
Loss of pigmentation over the shin area is not typically associated with peripheral venous disease. This symptom is more commonly seen in conditions such as chronic venous insufficiency (CVI), where prolonged venous hypertension leads to skin changes, including hyperpigmentation and lipodermatosclerosis. However, it is not a primary manifestation of PVD itself.
Choice C Reason:
A shiny appearance to the lower extremities is more commonly associated with peripheral arterial disease (PAD) rather than peripheral venous disease. In PAD, reduced blood flow to the extremities can cause the skin to become thin, shiny, and hairless. This is due to the lack of oxygen and nutrients reaching the skin and underlying tissues. In contrast, PVD primarily affects the veins and does not typically cause these skin changes.
Choice D Reason:
Diminished hair growth on the lower extremities is another symptom more commonly associated with peripheral arterial disease (PAD). In PAD, the reduced blood flow to the extremities can lead to hair loss, as the hair follicles do not receive adequate oxygen and nutrients. Peripheral venous disease, on the other hand, does not usually cause hair loss. Instead, it is characterized by symptoms related to venous insufficiency, such as varicose veins, swelling, and skin changes.
You just viewed 10 questions out of the 41 questions on the ATI Med Surg Final Exam Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



