Nur211 Mobility Exam
ATI Nur211 Mobility Exam
Total Questions : 35
Showing 10 questions Sign up for moreA nurse is monitoring a client who was admitted with a severe burn injury and is receiving IV fluid resuscitation therapy. The nurse should identify an increase in which of the following findings as an indication of adequate fluid replacement?
Explanation
Choice A Reason:
Urine output is one of the most reliable indicators of adequate fluid resuscitation in burn patients. The goal is to maintain a urine output of 0.5 to 1 mL/kg/hour in adults³. This parameter is crucial because it directly reflects renal perfusion and, by extension, overall circulatory volume status. When fluid resuscitation is adequate, the kidneys receive enough blood flow to produce urine at this rate, indicating that the body's tissues are being adequately perfused. Monitoring urine output is a non-invasive and straightforward method, making it a preferred choice in clinical settings.
Choice B Reason:
Heart rate can be an indicator of fluid status, but it is less reliable than urine output. Tachycardia (an increased heart rate) can occur due to pain, anxiety, or other stressors, not just fluid deficit. While a decreasing heart rate might suggest improving fluid status, it is not a definitive indicator on its own. Other factors must be considered in conjunction with heart rate to assess fluid resuscitation adequacy.
Choice C Reason:
Blood pressure is another parameter used to assess fluid status, but it can be influenced by many factors, including the patient's baseline blood pressure, medications, and the presence of other medical conditions. While maintaining adequate blood pressure is important, it is not as sensitive or specific as urine output for assessing fluid resuscitation in burn patients. Blood pressure can remain within normal ranges even when fluid resuscitation is inadequate, especially in the early stages.
Choice D Reason:
Mental status can be affected by fluid status, but it is a late indicator of inadequate perfusion. Changes in mental status, such as confusion or decreased level of consciousness, can occur when there is significant hypoperfusion and shock. By the time mental status changes are observed, the patient may already be in a critical state. Therefore, it is not a primary indicator for assessing fluid resuscitation adequacy.
Choice E Reason:
Capillary refill time is a quick and simple test to assess peripheral perfusion. However, it is not as reliable as urine output for evaluating overall fluid status. Capillary refill can be affected by ambient temperature, lighting conditions, and the examiner's technique. While a prolonged capillary refill time can indicate poor perfusion, it is not as specific or sensitive as urine output for assessing fluid resuscitation adequacy.
A nurse is caring for a client who has a closed-head injury with elevated ICP readings ranging from 16 to 22 mm Hg. Which of the following actions should the nurse take to decrease the potential for raising the client's ICP?
Explanation
Choice A Reason:
Elevating the client's head on two pillows can help reduce ICP by promoting venous drainage from the brain. However, it is important to ensure that the head is not elevated too high, as this can impede venous return and potentially increase ICP. The recommended elevation is typically 30 degrees. While this intervention is beneficial, it is not the most critical action compared to reducing environmental stimuli.
Choice B Reason:
Keeping the client well hydrated is essential for overall health, but excessive hydration can increase ICP by increasing the volume of cerebrospinal fluid and blood within the cranial vault. Fluid management must be carefully monitored to avoid exacerbating ICP. Therefore, while hydration is important, it must be balanced and not excessive.
Choice C Reason:
Decreasing the noise level in the client's room is crucial for minimizing external stimuli that can increase ICP. Noise and other environmental stressors can lead to increased agitation and stress, which in turn can elevate ICP. Creating a calm and quiet environment helps in maintaining a stable ICP and is a non-invasive, easily implementable intervention.
Choice D Reason:
Frequent suctioning of the endotracheal tube can cause transient increases in ICP due to the stimulation and potential for coughing. While suctioning is necessary to maintain airway patency, it should be performed judiciously and only when clinically indicated. Over-suctioning can lead to spikes in ICP and should be avoided.
Which of the following are types of shock and their respective causes? (Select All that Apply.)
Explanation
Choice A Reason:
Neurogenic shock occurs due to a disruption in the autonomic nervous system, often resulting from spinal cord injuries. This disruption leads to a loss of sympathetic tone, causing widespread vasodilation and a subsequent drop in blood pressure. The hallmark of neurogenic shock is hypotension with bradycardia, which differentiates it from other types of shock that typically present with tachycardia. The loss of vascular tone results in pooling of blood in the extremities, reducing venous return to the heart and decreasing cardiac output.
Choice B Reason:
Hypovolemic shock is caused by a significant loss of blood or fluids, leading to inadequate circulating volume. This can result from trauma, surgery, gastrointestinal bleeding, or severe dehydration. The primary mechanism is a reduction in preload, which decreases stroke volume and cardiac output. Clinical signs include tachycardia, hypotension, and cool, clammy skin. Rapid fluid resuscitation is critical to restore circulating volume and improve tissue perfusion.
Choice C Reason:
Metabolic shock is not a recognized type of shock in medical literature. The term might be confused with metabolic acidosis, which can occur secondary to shock but is not a primary cause. Metabolic acidosis results from the accumulation of lactic acid due to anaerobic metabolism when tissues are inadequately perfused. Therefore, metabolic shock is not considered a valid type of shock.
Choice D Reason:
Anaphylactic shock is a severe, life-threatening allergic reaction that leads to widespread vasodilation, increased capillary permeability, and bronchoconstriction. Common triggers include foods, insect stings, medications, and latex. Symptoms include hypotension, swelling, difficulty breathing, and hives. Immediate administration of epinephrine is crucial to counteract the severe allergic response and stabilize the patient.
Choice E Reason:
Septic shock results from a severe infection that leads to systemic inflammation and widespread vasodilation. The infection triggers an overwhelming immune response, causing damage to blood vessels and organs. Clinical features include fever, hypotension, tachycardia, and altered mental status. Early recognition and aggressive treatment with antibiotics and fluid resuscitation are essential to improve outcomes.
Choice F Reason:
Cardiogenic shock occurs when the heart fails to pump effectively, leading to inadequate tissue perfusion. Common causes include myocardial infarction, severe heart failure, and arrhythmias. Symptoms include hypotension, tachycardia, and signs of poor perfusion such as cool extremities and altered mental status. Treatment focuses on improving cardiac output through medications, mechanical support, or revascularization procedures.
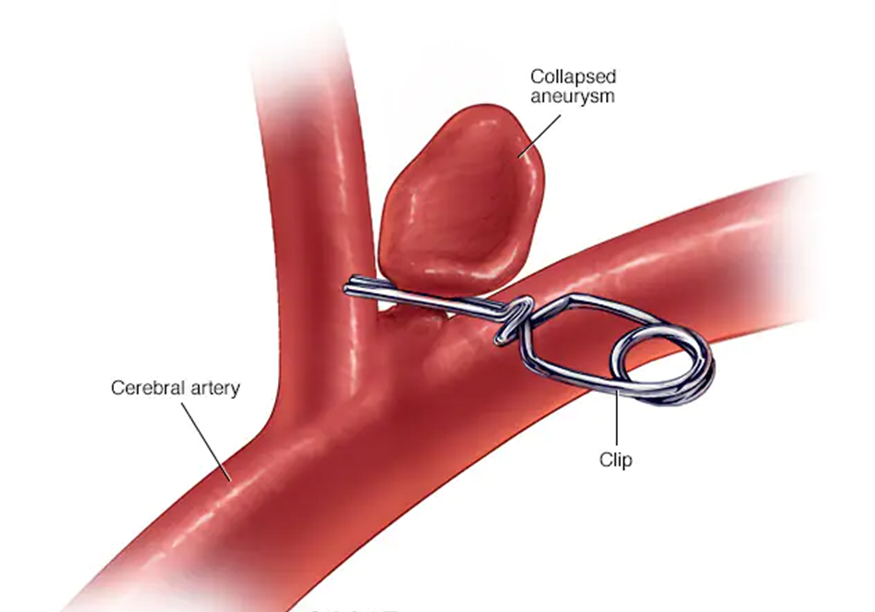
Which of the following is a potential complication of a treated aneurysm?
Explanation
Choice A Reason:
Improved blood flow to surrounding tissues is generally a desired outcome of treating an aneurysm, not a complication. When an aneurysm is successfully treated, the goal is to restore normal blood flow and prevent the aneurysm from rupturing. Improved blood flow indicates that the treatment was effective and that the risk of complications has been minimized.
Choice B Reason:
Rupture leading to severe internal bleeding is a significant potential complication of a treated aneurysm. Even after treatment, there is a risk that the aneurysm could rupture, especially if the treatment was not entirely successful or if the aneurysm was particularly large or complex. A rupture can lead to life-threatening internal bleeding and requires immediate medical attention. This is why ongoing monitoring and follow-up care are crucial for patients who have had an aneurysm treated.
Choice C Reason:
Decreased risk of blood clot formation is another desired outcome rather than a complication. Treating an aneurysm often involves measures to prevent blood clots, such as using anticoagulant medications. A successful treatment should reduce the risk of clot formation, which can otherwise lead to complications like stroke or embolism.
Choice D Reason:
Reduced risk of infection is also a desired outcome of aneurysm treatment. Infection can be a complication of any surgical procedure, including those used to treat aneurysms. However, with proper surgical techniques and post-operative care, the risk of infection can be minimized. Therefore, a reduced risk of infection is not a complication but rather an indication of successful treatment and good medical practice.
A nurse is monitoring the fluid replacement of a client who has sustained burns. The nurse should administer which of the following fluids in the first 24 hours following a burn injury?
Explanation
Choice A Reason:
0.9% sodium chloride is an isotonic crystalloid solution often used for fluid resuscitation. However, it is not the preferred choice for burn patients because it lacks the necessary electrolytes to replace those lost through burn injuries. While it can be used if Lactated Ringer's is unavailable, it does not provide the same balanced electrolyte composition.
Choice B Reason:
Lactated Ringer's is the preferred fluid for initial resuscitation in burn patients. It is an isotonic crystalloid solution that closely mimics the body's plasma, providing essential electrolytes such as sodium, potassium, calcium, and lactate. The lactate in the solution acts as a buffer, helping to correct metabolic acidosis, which is common in burn patients. The Parkland formula, widely used for calculating fluid needs in burn patients, specifically recommends Lactated Ringer's for the first 24 hours.
Choice C Reason:
Dextrose 5% in water is a hypotonic solution that provides free water and calories but lacks electrolytes. It is not suitable for initial fluid resuscitation in burn patients because it does not address the electrolyte imbalances and large fluid shifts that occur after a burn injury. Using this solution could lead to further complications such as hyponatremia.
Choice D Reason:
Dextrose 5% in 0.9% sodium chloride is a hypertonic solution that provides both glucose and electrolytes. However, it is not typically used for initial burn resuscitation because the high glucose content can lead to hyperglycemia, which is detrimental to burn patients. Additionally, the solution's osmolarity can exacerbate fluid shifts and worsen edema.
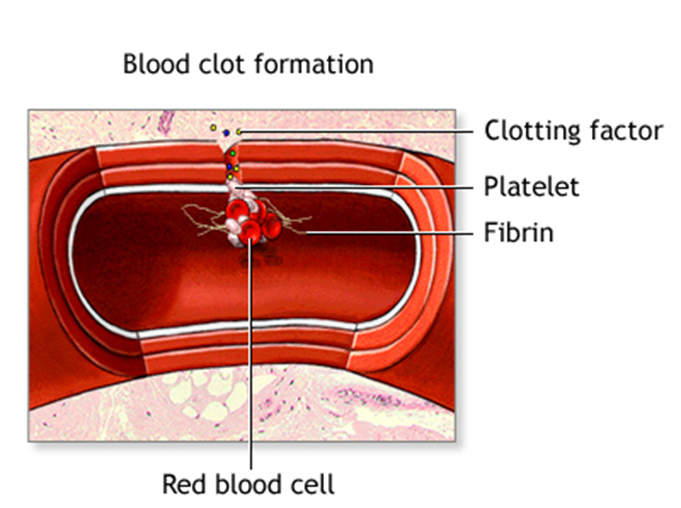
Which of the following are risk factors for disseminated intravascular coagulation (DIC)? (Select All that Apply.)
Explanation
Choice A Reason:
Cancer is a significant risk factor for DIC, particularly certain types of leukemia and metastatic cancers. Cancer can trigger DIC through the release of procoagulant substances from tumor cells, leading to widespread clotting and subsequent bleeding. The hypercoagulable state associated with malignancies increases the risk of thrombotic events, which can precipitate DIC. Patients with advanced cancer are particularly susceptible due to the aggressive nature of the disease and the body's inflammatory response.
Choice B Reason:
Sepsis is one of the most common causes of DIC. Sepsis triggers a systemic inflammatory response that activates the coagulation cascade, leading to the formation of microthrombi throughout the vasculature. This widespread clotting depletes clotting factors and platelets, resulting in a paradoxical increase in bleeding risk. The severity of sepsis correlates with the likelihood of developing DIC, making early recognition and treatment of sepsis crucial.
Choice C Reason:
Trauma can lead to DIC through extensive tissue injury and the release of tissue factor into the bloodstream. Severe trauma, such as that from major accidents or surgeries, can overwhelm the body's hemostatic mechanisms, leading to uncontrolled clotting and bleeding. The inflammatory response to trauma further exacerbates the coagulation process, increasing the risk of DIC. Prompt management of traumatic injuries and monitoring for signs of DIC are essential in these patients.
Choice D Reason:
Pregnancy complications such as placental abruption, amniotic fluid embolism, and severe preeclampsia can precipitate DIC. These conditions cause significant endothelial damage and the release of procoagulant substances, triggering the coagulation cascade. The physiological changes during pregnancy, including increased blood volume and hypercoagulability, further predispose pregnant women to DIC. Early intervention and management of pregnancy-related complications are vital to prevent DIC.
Choice E Reason:
Blood transfusion reactions can lead to DIC through immune-mediated mechanisms. Incompatible blood transfusions can cause hemolysis and the release of procoagulant substances, initiating the coagulation cascade. The resulting widespread clotting and consumption of clotting factors can lead to bleeding complications. Careful matching of blood products and monitoring for transfusion reactions are critical to prevent DIC in transfusion recipients.
The physician orders a Lidocaine drip to infuse at 2 mg/min. The drug is available as 2 gm in 500 mL of fluid. Solve for mL/hr.
Explanation
Step-by-Step Calculation:
Step 1: Convert 2 gm to mg.
2 gm × 1000 = 2000 mg
Step 2: Determine the concentration of Lidocaine in mg/mL.
2000 mg ÷ 500 mL = 4 mg/mL
Step 3: Calculate the infusion rate in mL/min.
2 mg/min ÷ 4 mg/mL = 0.5 mL/min
Step 4: Convert the infusion rate to mL/hr.
0.5 mL/min × 60 min/hr = 30 mL/hr
Result: The Lidocaine drip should be infused at 30 mL/hr.
A nurse in the emergency department is caring for a client who has extensive partial and full-thickness burns of the head. When planning the client's care, the nurse should identify which of the following risks as the priority for assessment and intervention:
Explanation
Choice A Reason:
Fluid imbalance is a significant concern in burn patients due to the loss of fluids through damaged skin. This can lead to hypovolemic shock if not managed properly. However, while fluid resuscitation is crucial, it is not the immediate priority over airway management in the case of burns to the head and neck. Ensuring the airway is clear and unobstructed takes precedence because airway compromise can lead to rapid deterioration and death.
Choice B Reason:
Airway obstruction is the most critical risk in patients with extensive burns to the head and neck. Burns in these areas can cause swelling, leading to airway compromise. Inhalation injuries from smoke or hot gases can also cause airway edema and respiratory distress. Immediate assessment and intervention to secure the airway are paramount to prevent hypoxia and ensure the patient can breathe adequately. This is why airway management is the top priority in such cases.
Choice C Reason:
Infection is a major risk for burn patients due to the loss of the skin barrier, which normally protects against pathogens. Burn wounds are highly susceptible to bacterial colonization and infection, which can lead to sepsis if not properly managed. While infection control is vital, it is not the immediate priority over securing the airway in the acute phase of burn management. Once the airway is secured, infection prevention and control measures can be implemented.
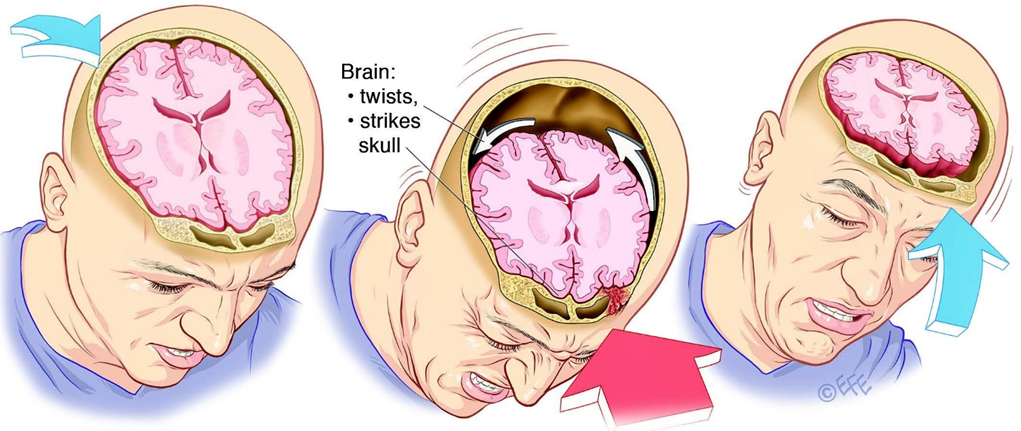
A nurse is caring for a client who has sustained a traumatic brain injury. The nurse should monitor the client for which of the following manifestations of increased intracranial pressure?
Explanation
Choice A Reason:
Hypotension is not typically a direct manifestation of increased intracranial pressure (ICP). In fact, increased ICP often leads to hypertension as part of Cushing's triad, which includes hypertension, bradycardia, and irregular respiration. Hypotension may indicate other issues such as shock or blood loss but is not a primary indicator of increased ICP.
Choice B Reason:
Tachypnea, or rapid breathing, is not a primary sign of increased ICP. While respiratory changes can occur with increased ICP, they are more likely to present as irregular breathing patterns rather than simply an increased rate. Tachypnea might be seen in conditions like anxiety, pain, or respiratory distress but is not a hallmark of increased ICP.
Choice C Reason:
Bilateral weakness of extremities can occur with increased ICP, especially if there is significant brain swelling or herniation affecting motor pathways. However, it is not the most immediate or specific sign. Other neurological deficits can also cause bilateral weakness, so it is not solely indicative of increased ICP.
Choice D Reason:
Decreased level of consciousness is a critical and primary sign of increased ICP. As pressure within the skull rises, it can compress brain structures and impair function, leading to altered mental status ranging from confusion to coma. Monitoring the level of consciousness is essential in assessing and managing patients with potential increased ICP.
Which of the following are types of infections that can affect the ear? (Select All that Apply.)
Explanation
Choice A Reason:
Pneumonia is an infection of the lungs, not the ear. It primarily affects the alveoli, causing symptoms like cough, fever, and difficulty breathing. While respiratory infections can sometimes lead to ear infections, pneumonia itself does not directly infect the ear.
Choice B Reason:
Endocarditis is an infection of the inner lining of the heart chambers and valves. It is typically caused by bacteria entering the bloodstream and does not affect the ear. Symptoms include fever, heart murmurs, and fatigue.
Choice C Reason:
Myocarditis is an inflammation of the heart muscle, usually caused by viral infections. It affects the heart's ability to pump blood and does not involve the ear. Symptoms can include chest pain, fatigue, and shortness of breath.
You just viewed 10 questions out of the 35 questions on the ATI Nur211 Mobility Exam Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



