Paediatrics Exam 2
ATI Paediatrics Exam 2
Total Questions : 66
Showing 10 questions Sign up for moreA nurse is caring for an 18-month-old toddler in the emergency department. The nurse reviews the toddler's medical record and assessment findings. Which of the following provider prescriptions should the nurse anticipate?
Explanation
Choice A reason: Acetaminophen suppository is not a likely prescription, as it is used to reduce fever and pain, which are not the main problems of the toddler. The toddler has a high axillary temperature of 39.5°C (103.1°F), which is not considered a fever in children under 2 years old. The normal axillary temperature range for children is 36.5°C to 37.5°C (97.7°F to 99.5°F).
Choice B reason: Oral rehydration solution is not a probable prescription, as it is used to prevent or treat dehydration caused by diarrhea, vomiting, or excessive sweating, which are not the main problems of the toddler. The toddler has a normal respiratory rate of 22/min and oxygen saturation of 98%, which indicate adequate hydration and oxygenation.
Choice C reason: Nebulized albuterol is a possible prescription, as it is used to treat bronchospasm, which is a common complication of respiratory infections in children. The toddler has a high apical heart rate of 142/min, which may indicate respiratory distress or hypoxia. The toddler is also pulling at his ear, which may indicate an ear infection or pain.
Choice D reason: Intravenous antibiotics are not a likely prescription, as they are used to treat bacterial infections, which are not the main problems of the toddler. The toddler has no signs or symptoms of a bacterial infection, such as purulent discharge, foul odor, or localized inflammation. The toddler may have a viral infection, which does not respond to antibiotics.
Explanation
Choice A reason: Intravenous immunoglobulin is a likely prescription, as it is used to treat Kawasaki disease, which is a rare but serious condition that causes inflammation of the blood vessels in children. The toddler has many signs and symptoms of Kawasaki disease, such as high fever, irritability, red eyes, dry lips, strawberry tongue, swollen hands and feet, rash, and enlarged lymph node. Intravenous immunoglobulin can reduce the risk of complications, such as coronary artery aneurysms, which can be life-threatening.
Choice B reason: Oral acyclovir is not a probable prescription, as it is used to treat viral infections, such as herpes simplex or varicella zoster, which are not the main problems of the toddler. The toddler has no evidence of a viral infection, such as blisters, vesicles, or crusts.
Choice C reason: Intramuscular penicillin is not a likely prescription, as it is used to treat bacterial infections, such as streptococcal pharyngitis or syphilis, which are not the main problems of the toddler. The toddler has no signs of a bacterial infection, such as purulent discharge, foul odor, or localized inflammation.
Choice D reason: Topical hydrocortisone is not a helpful prescription, as it is used to treat skin conditions, such as eczema or dermatitis, which are not the main problems of the toddler. The toddler has a rash that is caused by the inflammation of the blood vessels, not by an allergic or irritant reaction. Topical hydrocortisone may also worsen the rash or cause skin thinning or infection.
Explanation
Choice A reason: Continuing to monitor the client is not the best action, as it does not address the low urine output of the child. The child has a urine output of 20 mL/hr, which is below the expected range of 30 to 40 mL/hr for a 3-year-old child. Low urine output can indicate dehydration, kidney injury, or urinary tract obstruction, which require prompt intervention.
Choice B reason: Performing a bladder scan at the bedside is not the most appropriate action, as it is not the first-line diagnostic tool for low urine output. A bladder scan is a noninvasive ultrasound device that measures the amount of urine in the bladder. It can help detect urinary retention, which is the inability to empty the bladder completely. However, urinary retention is unlikely in a 3-year-old child, and a bladder scan may not be accurate or reliable in children.
Choice C reason: Providing oral rehydration fluids is the best action, as it can help restore the fluid and electrolyte balance of the child. Oral rehydration fluids are solutions that contain water, sugar, and salt in specific proportions that match the body's needs. They can prevent or treat dehydration, which is a common cause of low urine output in children. The nurse should offer the child oral rehydration fluids every 15 to 20 minutes, and monitor the urine output, vital signs, and hydration status.
Choice D reason: Notifying the provider is not the first action, as it is not the most urgent or effective intervention for low urine output. The nurse should notify the provider after providing oral rehydration fluids and assessing the child's response. The nurse should also report any signs or symptoms of dehydration, such as dry mucous membranes, sunken eyes, poor skin turgor, or lethargy. The provider may order further tests or treatments, such as blood tests, urine tests, or intravenous fluids.
Explanation
Choice A reason: Rice is a suitable food choice for a child who has celiac disease, as it is a gluten-free grain that does not cause inflammation or damage to the small intestine. Rice can provide carbohydrates, fiber, and vitamins for the child's nutrition.
Choice B reason: Rye is not a good food choice for a child who has celiac disease, as it is a gluten-containing grain that can trigger an immune response and harm the small intestine. Rye can cause symptoms such as diarrhea, abdominal pain, bloating, and weight loss in the child.
Choice C reason: Wheat is not a good food choice for a child who has celiac disease, as it is a gluten-containing grain that can trigger an immune response and harm the small intestine. Wheat can cause symptoms such as diarrhea, abdominal pain, bloating, and weight loss in the child.
Choice D reason: Barley is not a good food choice for a child who has celiac disease, as it is a gluten-containing grain that can trigger an immune response and harm the small intestine. Barley can cause symptoms such as diarrhea, abdominal pain, bloating, and weight loss in the child.
Explanation
Choice A reason: Maintaining the infant in the supine position is not an appropriate intervention, as it can increase the pressure on the myelomeningocele sac and cause further damage to the spinal cord. The nurse should position the infant prone or side-lying, with the head turned to one side and the hips flexed.
Choice B reason: Limiting visitors to immediate family members is not a necessary intervention, as the infant does not have an infectious condition that requires isolation. The nurse should encourage the parents and other family members to visit and bond with the infant, and provide emotional support and education.
Choice C reason: Initiating contact precautions is not a required intervention, as the infant does not have a contagious condition that poses a risk of transmission to others. The nurse should follow standard precautions, such as washing hands, wearing gloves, and disposing of contaminated materials properly.
Choice D reason: Providing a latex-free environment is an essential intervention, as the infant has a high risk of developing a latex allergy due to the frequent exposure to latex products during surgery and other procedures. The nurse should avoid using latex gloves, catheters, syringes, bandages, or other items that contain latex, and use alternative materials instead. The nurse should also label the infant's chart, crib, and door with a latex allergy alert.
The nurse is caring for a 4-month-old infant in the emergency department. The nurse reviews the infant's medical record and assessment findings. Which of the following conditions should the nurse suspect, and what actions should the nurse take to address that condition, and what parameters should the nurse monitor to assess the infant's progress?
The nurse should suspect that the infant has
Explanation
Choice A reason: Meningitis is a possible condition, as it is an inflammation of the membranes that cover the brain and spinal cord. It can be caused by various microorganisms, such as bacteria, viruses, or fungi. The infant has many signs and symptoms of meningitis, such as fever, irritability, lethargy, bulging fontanel, and clear cerebrospinal fluid from the lumbar puncture.
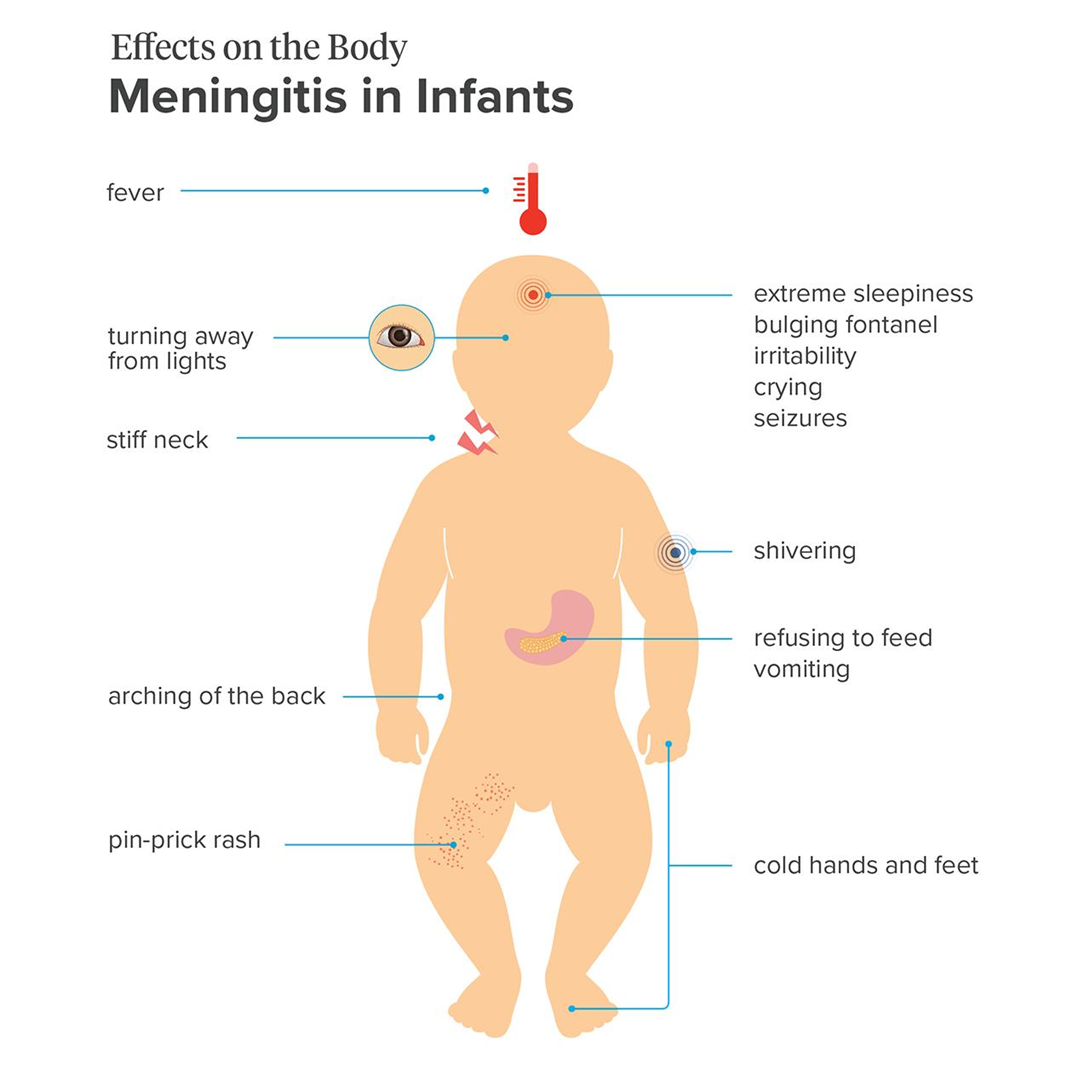
Choice B reason: Hydrocephalus is not a likely condition, as it is an accumulation of cerebrospinal fluid in the brain, which causes increased intracranial pressure and enlargement of the head. The infant has a bulging fontanel, which can indicate increased intracranial pressure, but not necessarily hydrocephalus. The infant does not have other signs of hydrocephalus, such as a rapidly increasing head circumference, prominent scalp veins, or sunset eyes.
Choice C reason: Intracranial hemorrhage is not a probable condition, as it is a bleeding within the skull, which can result from trauma, vascular malformation, or coagulation disorder. The infant has retinal hemorrhages, which can indicate intracranial hemorrhage, but not necessarily. The infant does not have other signs of intracranial hemorrhage, such as seizures, vomiting, or altered mental status.
Choice D reason: Sepsis is not a definite condition, as it is a systemic inflammatory response to an infection, which can cause organ dysfunction and shock. The infant has a fever, which can indicate sepsis, but not necessarily. The infant does not have other signs of sepsis, such as tachycardia, tachypnea, hypotension, or poor perfusion.
The nurse should suspect that the infant has
Explanation
Choice A reason: Failure to thrive is not a likely condition, as it is a term used to describe inadequate growth or weight gain in children. The infant has a low weight percentile, but not below the 5th percentile, which is the usual cutoff for failure to thrive. The infant's length and head circumference are within the normal range, which also does not indicate failure to thrive.
Choice B reason: Microcephaly is not a probable condition, as it is a condition where the head size is much smaller than normal for the age and sex of the child. The infant has a high head circumference percentile, which is the opposite of microcephaly. Microcephaly can be caused by genetic disorders, infections, or brain damage.
Choice C reason: Hydrocephalus is a possible condition, as it is a condition where excess cerebrospinal fluid accumulates in the brain, causing increased pressure and enlargement of the head. The infant has a high head circumference percentile, which can indicate hydrocephalus. The infant also has a low weight percentile, which can be a result of poor feeding or vomiting due to increased intracranial pressure. T
Choice D reason: Macrocephaly is not a definite condition, as it is a term used to describe a head size that is much larger than normal for the age and sex of the child. The infant has a high head circumference percentile, but not above the 97th percentile, which is the usual cutoff for macrocephaly. Macrocephaly can be caused by genetic factors, benign familial macrocephaly, or other conditions, such as hydrocephalus.
Explanation
Choice A reason: The child has acute lymphoblastic leukemia (ALL) and is receiving chemotherapy and steroids, which can cause constipation. The nurse should monitor the child's bowel function and provide interventions such as fluids, fiber, and laxatives as prescribed, but this is not an urgent finding.
Choice B reason: The child is in the induction phase of treatment for ALL, which can be stressful and frightening for the child and the family. The child's crying and clinging behavior indicates anxiety and fear, which are normal reactions. The nurse should provide emotional support and education to the child and the guardian, but this is not an urgent finding.
Choice C reason: The child has a fever, which is a common side effect of chemotherapy and steroids. The nurse should assess the child for other signs of infection, administer antipyretics as prescribed, and monitor the child's vital signs, but this is not an urgent finding.
Choice D reason: The child has a double-lumen central line catheter in the left chest wall, which is a potential source of infection. The erythema and purulent drainage at the insertion site indicate that the child has a local infection, which can spread to the bloodstream and cause sepsis. This is a life-threatening complication that requires immediate attention and treatment. The nurse should report this finding to the provider, obtain blood cultures, and administer antibiotics as prescribed.
- WBC count 15,000/mm^3^ (normal range: 5,000 to 10,000/mm^3^)
- Hgb 8 g/dL (normal range: 10 to 15.5 g/dL)
- Hct 32% (normal range: 32% to 44%)
The nurse should suspect that the child has which of the following conditions?
Explanation
Choice A reason: Leukemia is not a probable condition, as it is a cancer of the white blood cells that causes abnormal proliferation and accumulation of immature or dysfunctional white blood cells. The child has a high WBC count, which can indicate leukemia, but not necessarily. The child does not have other signs of leukemia, such as bleeding, bruising, bone pain, or lymphadenopathy.
Choice B reason: Sickle cell anemia is a possible condition, as it is an inherited disorder that affects the shape and function of the red blood cells, causing them to become sickle-shaped and rigid. The child has a low Hgb and Hct, which can indicate anemia, and a fever, tachycardia, and low oxygen saturation, which can indicate a sickle cell crisis. A sickle cell crisis is a condition where the sickle-shaped red blood cells block the blood flow and cause tissue ischemia and inflammation.
Choice C reason: Hemophilia is not a likely condition, as it is an inherited disorder that affects the clotting factors, causing impaired blood clotting and increased risk of bleeding. The child has a low Hgb and Hct, which can indicate anemia, but not necessarily hemophilia. The child does not have other signs of hemophilia, such as bleeding, bruising, hemarthrosis, or hematuria.
Choice D reason: Iron deficiency anemia is not a definite condition, as it is a type of anemia that occurs when the body does not have enough iron to produce hemoglobin, the protein that carries oxygen in the blood. The child has a low Hgb and Hct, which can indicate iron deficiency anemia, but not necessarily. The child does not have other signs of iron deficiency anemia, such as pallor, fatigue, weakness, or pica.
Explanation
Choice A reason: A 2-year-old toddler is not a recommended recipient of the MCV4 vaccine, as it is not routinely given to children younger than 11 years old, unless they have certain medical conditions that increase their risk of meningococcal disease, such as asplenia, complement deficiency, or HIV infection. A 2-year-old toddler may receive the meningococcal polysaccharide (MPSV4) vaccine instead, if indicated.
Choice B reason: A 4-month-old infant is not a recommended recipient of the MCV4 vaccine, as it is not routinely given to children younger than 11 years old, unless they have certain medical conditions that increase their risk of meningococcal disease, such as asplenia, complement deficiency, or HIV infection. A 4-month-old infant may receive the meningococcal serogroup B (MenB) vaccine instead, if indicated.
Choice C reason: An 11-year-old school-age child is a recommended recipient of the MCV4 vaccine, as it is routinely given to children aged 11 to 12 years old, with a booster dose at age 16. The MCV4 vaccine protects against four types of meningococcal bacteria (A, C, W, and Y) that can cause serious infections of the lining of the brain and spinal cord (meningitis) or the bloodstream (septicemia).
Choice D reason: A 4-year-old child is not a recommended recipient of the MCV4 vaccine, as it is not routinely given to children younger than 11 years old, unless they have certain medical conditions that increase their risk of meningococcal disease, such as asplenia, complement deficiency, or HIV infection. A 4-year-old child may receive the meningococcal polysaccharide (MPSV4) vaccine instead, if indicated.
You just viewed 10 questions out of the 66 questions on the ATI Paediatrics Exam 2 Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



